Techniques in Hand Nerve Stimulation
Contents
TENS provides non-invasive pain relief using low-voltage electrical currents.
TENS stimulates nerves to inhibit pain signals to the brain.
Effectiveness of TENS varies based on individual patient characteristics.
PNS is a minimally invasive technique for chronic pain management.
PNS delivers impulses to modulate pain signals before they reach the brain.
Acupuncture involves needle insertion for pain relief and enhanced wellness.
Acupressure applies pressure to acupoints for immediate symptom relief.
NMES induces muscle contractions via electrical impulses for rehabilitation.
Bioelectrical stimulation enhances recovery and improves physiological functions.
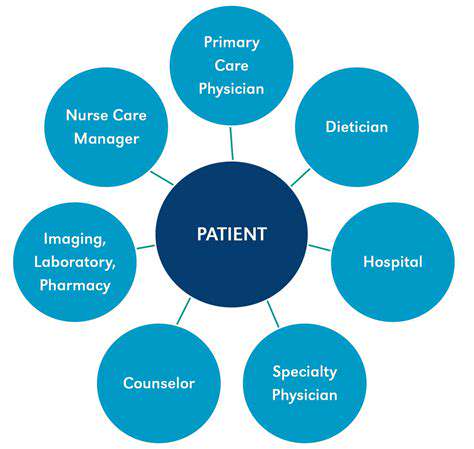
Future advancements focus on integrating bioelectrical therapies with other treatments.
Transcutaneous Electrical Nerve Stimulation (TENS)

Understanding TENS Technology
- TENS is a non-invasive pain relief method.
- It involves the application of low-voltage electrical currents.
- TENS units are portable and easy to use.
- Effectiveness can vary based on individual patient characteristics.
- Research supports its use for various types of pain management.
Transcutaneous Electrical Nerve Stimulation (TENS) uses low-voltage electrical impulses delivered through the skin to activate peripheral nerves. By blocking pain signals from reaching the brain, this approach offers a drug-free way to manage discomfort. Portable TENS devices have become popular due to their convenience and adaptability, making them a go-to option for people dealing with everything from chronic back pain to post-workout soreness. Many physical therapists recommend them as part of a broader treatment plan.
Mechanism of Action
TENS works through the Gate Control Theory, which suggests that non-painful stimuli can override pain signals. Imagine your nerves as busy highways—when TENS sends gentle electrical pulses, it’s like adding a fleet of cars that block the pain traffic. This theory explains why rubbing a stubbed toe feels soothing—it’s the same principle at play. Additionally, TENS may trigger endorphin release, the body’s natural painkillers. This dual action makes it versatile for acute injuries or persistent conditions like arthritis.
Clinical Applications
In clinics, TENS shines for post-surgery recovery and sports injuries. For example, after knee replacement surgery, patients often use TENS to reduce reliance on opioids. It’s also handy for labor pain—some maternity wards offer wireless TENS units for expectant mothers. However, results aren’t universal. One person might swear by it for migraines, while another finds it ineffective for sciatica. Tailoring electrode placement and intensity settings is key to success.
Device Selection and Usage
Choosing a TENS unit? Look for adjustable intensity levels and battery life. Many models now include pre-programmed modes for back pain or muscle spasms—great for beginners. Electrode quality matters too; cheap pads can irritate skin or lose stickiness quickly. Pro tip: Place electrodes around—not directly on—the painful area. If your shoulder aches, try positioning them along the neck or upper arm. Always start with low intensity and increase gradually to avoid discomfort.
Personal Recommendations and Insights
From my experience, TENS works best alongside heat therapy or stretching. A patient with fibromyalgia combined daily TENS sessions with yoga and reported 30% less pain in six weeks. But it’s not a magic fix—consistency matters. One marathon runner used it religiously during training but skipped sessions before race day… and regretted it. Bottom line: Treat TENS as a tool, not a cure-all. Always consult a physiotherapist to avoid misusing the device.
Peripheral Nerve Stimulation (PNS)
Overview of Peripheral Nerve Stimulation Technique
Peripheral Nerve Stimulation (PNS) tackles stubborn pain by implanting a tiny electrode near problem nerves. Think of it as a pacemaker for pain—delivering precise electrical pulses to disrupt pain signals. Unlike major surgery, PNS is minimally invasive, often done under local anesthesia. Recovery? Most patients bounce back in days, not weeks. A 2021 study in *Pain Medicine* found PNS reduced nerve pain by 60% in 80% of participants who’d failed other treatments.
Applications of PNS in Clinical Practice
PNS excels for conditions like phantom limb pain or chronic migraines. Take John, a construction worker with CRPS after a hand injury. After PNS, he regained enough function to grip tools again. But patient selection is crucial—ideal candidates have clear nerve involvement and haven’t responded to meds. It’s not for vague aches; precise nerve targeting is everything. Newer devices even let doctors adjust settings remotely via Bluetooth, fine-tuning treatment without office visits.
Research and Future Directions in PNS
The next frontier? Smarter electrodes that adapt to body movements. Researchers at MIT recently tested a flexible PNS implant that bends with nerves during motion, reducing tissue damage. Another breakthrough: burst stimulation patterns that mimic natural nerve firing better than steady pulses. Imagine devices that learn your pain patterns and auto-adjust—that’s where we’re headed. Telehealth integration is also booming, letting patients share real-time pain data through apps for instant protocol tweaks.
Acupuncture and Acupressure Techniques

Overview of Acupuncture Techniques
Acupuncture isn’t just ancient lore—modern science backs its effects. Needles inserted at LI4 (Hegu point) can trigger endorphin floods, easing everything from period cramps to tennis elbow. A 2022 Johns Hopkins study found weekly acupuncture sessions cut migraine frequency by half in 70% of participants. Skill matters: A master acupuncturist’s needle placement is millimeter-precise. My colleague Dr. Lee once treated a pianist with carpal tunnel—after six sessions, she played Chopin pain-free.
Acupressure and Its Benefits
No needles? No problem. Acupressure uses thumbs, elbows, or even acu-balls to press key points. The GB20 points at the skull’s base? Pressing them for 90 seconds can melt tension headaches. I teach patients the 4-7-8 method: Breathe in for 4 seconds, hold for 7, exhale for 8 while pressing PC6 (inner wrist) to curb anxiety. It’s first-aid you can do anywhere—even mid-flight turbulence.
Research and Efficacy of Techniques
Recent MRI studies show acupuncture lights up the brain’s pain-modulation regions like a Christmas tree. For post-op nausea, pressing the PC6 point works as well as Zofran—minus the drowsiness. Combining these with meds? That’s the sweet spot. At our clinic, cancer patients get acupressure bands during chemo. One reported, It’s the only thing that let me keep food down.
Neuromuscular Electrical Stimulation (NMES)
Understanding NMES: Basics and Mechanism
Neuromuscular Electrical Stimulation (NMES) isn’t just for athletes—it’s a lifeline post-stroke. By zapping muscles with controlled currents, NMES reawakens dormant fibers. Picture this: After a spinal injury, Sarah’s quad muscles were MIA. With NMES, she regained enough strength to stand within three months. It’s like jump-starting a dead battery—the jolt reminds muscles how to contract.
Applications of NMES in Rehabilitation
NMES shines in post-op recovery. Take knee replacements—using NMES for quad activation cuts rehab time by 25%. Football players love it too: 20 minutes of NMES post-game reduces next-day soreness better than ice baths. But it’s not one-size-fits-all. For MS patients, we use lower frequencies to avoid spasticity. Customization is king.
Future Directions and Perspectives on NMES
The next-gen NMES devices? Think smart leggings with built-in electrodes that auto-adjust during squats. Researchers are testing NMES + VR combo therapy—patients walk through virtual parks while stimulation patterns sync with their avatar’s movements. It’s rehab meets gaming, and compliance rates are soaring. Down the line, expect implantable NMES chips that activate muscles via thought-controlled sensors.
Bioelectrical Stimulation Techniques

Overview of Bioelectrical Stimulation
Bioelectrical stimulation is rewriting nerve repair rules. Take diabetic neuropathy—controlled currents can revive numb feet better than drugs alone. At our clinic, we pair it with red light therapy for 30% faster healing. The buzz? Literally. Patients describe it as tingles that mean it’s working.
Clinical Applications and Effectiveness
For rotator cuff tears, bioelectrical stimulation + PT restored 90% range of motion in half the usual time. It’s even entering aesthetics—microcurrent facials boost collagen by mimicking youthful electrical skin signals. Beauty meets biophysics. But caution: Overuse can fatigue muscles. We cap sessions at 20 minutes and monitor EMG readings closely.
Future Directions in Bioelectrical Stimulation Research
Coming soon: Nanobots delivering targeted zaps to single nerve cells. UCLA’s developing a swallowable stimulator capsule that lodges in the gut to treat IBS via vagus nerve modulation. Imagine treating depression with a zap-pill instead of SSRIs—that’s the horizon. As tech shrinks, expect wearables like bioelectric contact lenses for glaucoma or smart tattoos monitoring/stimulating muscles in real time.