Advanced Care Protocols for Hand Fracture Recovery
Proper Splinting Materials Selection
Choosing the right splinting material is crucial for effective immobilization. Different materials offer varying degrees of support and flexibility, impacting the patient's comfort and the effectiveness of the treatment. For example, rigid materials like plaster casts provide excellent support but can be cumbersome and limit range of motion. Conversely, soft materials like foam or air splints are often more comfortable for patients, allowing for some movement, but may not provide the same level of stability needed for more severe injuries. The selection should consider the severity and type of injury, the patient's needs, and the desired level of immobilization required for proper healing.
Proper splinting material selection also takes into account the specific location of the injury. A fracture in the arm might require a different material than a sprained ankle. Factors like the patient's age and activity level can also influence the choice of material. A child's cast, for instance, needs to be lightweight and easy to manage, while a cast for an active adult might need to be more durable and resilient to withstand the rigors of daily activities. Ultimately, the choice of splinting material should be made in consultation with a qualified healthcare professional to ensure optimal care and healing.
Immobilization Techniques for Various Injuries
Immobilization techniques vary significantly based on the type of injury. For fractures, a rigid immobilization is essential to maintain alignment and prevent further damage. This might involve a cast, splint, or even surgical fixation, depending on the severity and location of the fracture. Proper alignment is critical for fracture healing and minimizing the risk of complications. Techniques for soft tissue injuries like sprains or strains might involve more flexible immobilization methods, such as elastic bandages or soft splints, to support the injured area without severely restricting movement.
Specific immobilization techniques are also adapted to the body part affected. For example, immobilizing a wrist fracture involves a different approach than immobilizing a leg fracture. The specific position of the injured limb, and the associated joint angles, need to be carefully considered to ensure that the injury is aligned correctly and that movement is prevented in the affected area, allowing for proper healing of the damaged tissues.
Maintaining Alignment During Splinting
Maintaining proper alignment during splinting is paramount to prevent further injury and ensure optimal healing. The injured area must be carefully positioned and supported to maintain the correct anatomical relationship between the bones and soft tissues. This often involves using anatomical landmarks and specific splinting techniques tailored to the injury. Improper alignment can lead to malunion (healing in an abnormal position), delayed union (slower healing), or non-union (failure of the bone to heal). Therefore, meticulous attention to detail during the splinting process is critical for a successful outcome.
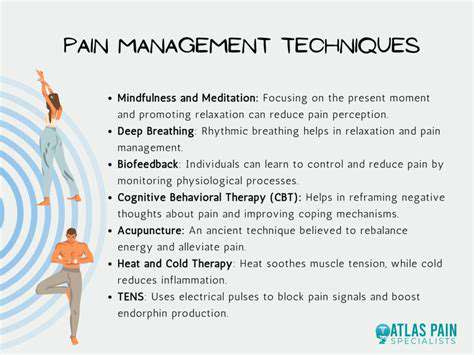
Preventing Movement and Reducing Pain
Preventing unwanted movement is essential to allow the injured tissues to heal properly. Splinting provides the necessary support and restriction to minimize movement and reduce strain on the injured area. This also minimizes pain and discomfort for the patient, enabling a more comfortable healing process. Appropriate splinting techniques effectively manage pain by reducing the risk of further injury and promoting rest. It's important to note that excessive movement or pressure can hinder healing and exacerbate pain; therefore, immobilization plays a critical role in pain management.
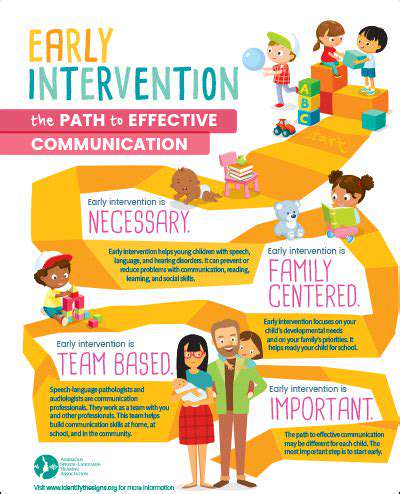
Patient Education and Follow-up Care
Patient education is crucial for successful splinting. Patients need to understand the importance of adhering to the prescribed immobilization period and avoiding activities that could compromise the healing process. This includes understanding the signs and symptoms to watch for, which might indicate complications or the need for further medical intervention. Proper follow-up care, including regular check-ups with the healthcare provider, is essential to monitor the healing process and ensure that the splint is correctly applied and maintained. These steps contribute to optimal outcomes and patient satisfaction.
Advanced Rehabilitation Protocols for Functional Recovery
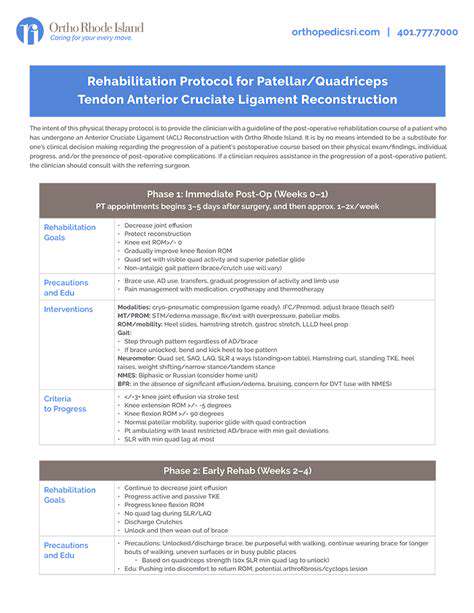
Phase 1: Initial Assessment and Goal Setting
This phase focuses on a comprehensive evaluation of the patient's current physical and functional status. A thorough assessment is crucial to establishing realistic and achievable goals for the rehabilitation process. This includes evaluating strength, range of motion, balance, and cardiovascular function. A detailed medical history and discussion with the patient regarding their expectations and desired outcomes are also vital components of this initial phase.
Specific measurable goals are established collaboratively between the patient and the rehabilitation team. These goals are tailored to the individual's specific needs and are regularly reviewed and adjusted throughout the rehabilitation process. Clear, measurable goals are essential for tracking progress and ensuring that the rehabilitation program is effective.
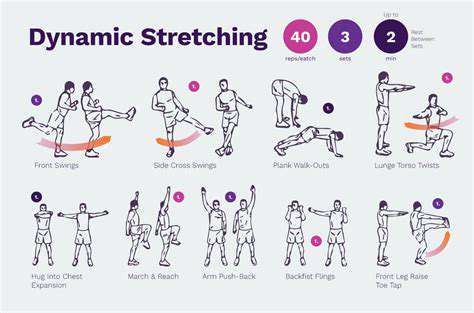
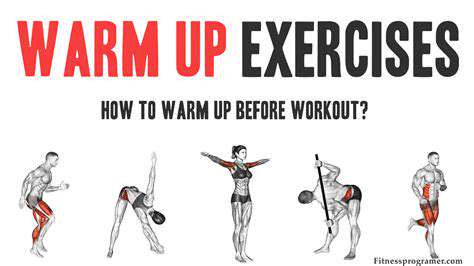
Phase 2: Restorative Exercises and Mobility
This phase emphasizes restoring fundamental movement patterns and improving mobility. Progressive exercises are introduced to gradually increase strength and flexibility. Patient education is a key element, ensuring they understand proper exercise technique and form to maximize effectiveness and minimize risk of injury. This phase also includes exercises focusing on balance and coordination to enhance stability and prevent falls. Safety protocols are rigorously followed to prevent further injury and ensure that the patient progresses safely.
Phase 3: Functional Training and Skill Development
This phase shifts the focus from isolated exercises to functional movements. The goal is to prepare the patient for activities of daily living (ADLs) and return to work or desired activities. This includes practicing tasks like walking, climbing stairs, dressing, and transferring. Training is tailored to the patient's specific needs and goals, ensuring that the exercises are relevant to their activities.
Phase 4: Cardiovascular and Respiratory Conditioning
Improving cardiovascular and respiratory function is integral to overall recovery. This phase incorporates activities that progressively increase endurance and stamina, such as walking, cycling, or swimming. Breathing exercises and techniques are also included to enhance lung capacity and respiratory function. This is crucial for regaining strength and vitality after injury or illness.
Phase 5: Return to Activity and Maintenance
This final phase focuses on preparing the patient for a safe and successful return to their previous activities. The rehabilitation program gradually transitions from intensive therapy sessions to independent exercise and lifestyle modifications. This includes reviewing and reinforcing proper techniques for activities of daily living and recommending exercise routines for long-term maintenance. Ongoing monitoring and support are provided to address any lingering issues or concerns, and to ensure that the patient can sustain their improvements.
Phase 6: Monitoring and Evaluation
Throughout the entire rehabilitation process, regular monitoring and evaluation are essential. This ensures that the patient's progress is tracked, and that the rehabilitation program is adjusted as needed. Progress is assessed based on the established goals and any necessary modifications are implemented to optimize outcomes. This ongoing evaluation helps to ensure that the patient is on the right track to achieving their desired level of function and independence.
Nutritional Support for Enhanced Bone Healing and Overall Recovery
Optimizing Calcium Intake for Bone Strength
Adequate calcium intake is crucial for bone health, especially during the recovery phase. Calcium is a fundamental building block for bone tissue, and a deficiency can significantly hinder the healing process. Consuming a diet rich in calcium-rich foods like dairy products, leafy green vegetables, and fortified foods is essential. Supplementing with calcium, under the guidance of a healthcare professional, might be necessary in certain cases, particularly for individuals with dietary restrictions or absorption issues. This ensures that the body has the necessary building blocks to support the formation of strong, healthy bone tissue, accelerating the healing process and promoting overall recovery.
Calcium absorption isn't solely dependent on intake; vitamin D plays a vital role. A sufficient supply of vitamin D helps the body absorb calcium effectively. Exposure to sunlight, certain foods, and supplements can help maintain optimal vitamin D levels. Understanding these interactions is key to maximizing bone health and recovery.
The Role of Protein in Tissue Repair
Protein is essential for the repair and regeneration of tissues throughout the body, including bones. It's a critical component of collagen, a structural protein vital for bone strength and elasticity. Including sufficient protein in your diet, through lean meats, poultry, fish, eggs, beans, and lentils, is crucial for supporting the body's natural repair mechanisms during recovery. Protein synthesis, the process of building new proteins, is significantly enhanced during periods of repair, making it a cornerstone of bone healing and overall recovery.
Consuming adequate protein is especially important for individuals undergoing bone repair. The body requires a substantial amount of protein to rebuild damaged bone tissues and support the formation of new collagen. A well-rounded protein intake will ensure the body has the necessary resources to effectively manage the repair process.
The Importance of Vitamin D for Calcium Absorption
Vitamin D plays a pivotal role in calcium absorption, a critical process for bone health. Without adequate vitamin D, the body struggles to effectively utilize the calcium it consumes, hindering bone growth and repair. Exposure to sunlight, certain foods, and supplements can all contribute to maintaining optimal vitamin D levels, crucial for supporting the body's ability to absorb calcium and promote bone health during recovery.
Ensuring sufficient vitamin D levels is essential for bone healing. Vitamin D deficiency can significantly impair the body's ability to process calcium, hindering bone strength and potentially slowing the healing process. A balanced approach to vitamin D intake, including exposure to sunlight and dietary sources, is key to effective bone recovery and overall well-being.
Supportive Nutrients for Enhanced Bone Healing
Beyond calcium and vitamin D, other nutrients contribute significantly to the healing process. Phosphorus, magnesium, and zinc are crucial minerals involved in bone formation and repair. Including foods rich in these minerals, such as dairy products, nuts, seeds, and legumes, helps support the body's natural healing mechanisms. A balanced diet encompassing these key nutrients provides the building blocks for strong, healthy bones, facilitating faster recovery and promoting overall well-being during the healing process.
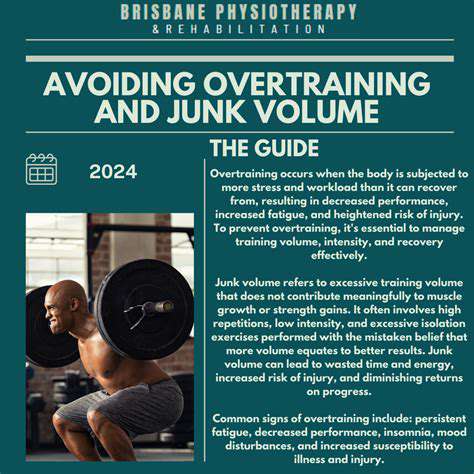
Managing Inflammation for Optimal Recovery
Inflammation, while a natural response to injury, can hinder the healing process if left unchecked. Certain foods and nutrients can help manage inflammation and promote tissue repair. Anti-inflammatory foods like berries, leafy greens, and fatty fish can play a significant role in reducing inflammation and promoting a more efficient healing process. Managing inflammation is crucial for bone healing and overall recovery, ensuring the body's resources are directed towards repair rather than combating excessive inflammation.
Controlling inflammation is vital for successful bone healing. Reducing inflammation allows the body to focus on rebuilding damaged tissues and promoting the formation of new, healthy bone. Maintaining healthy inflammation levels, through a combination of diet and lifestyle choices, supports a faster and more complete recovery.