Empowering Hand Rehabilitation via Physical Therapy
Index
- Customized physical therapy programs significantly improve the recovery outcomes of hand injuries
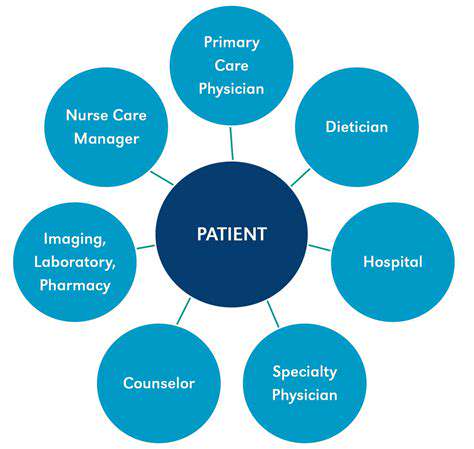
- The shortage of professional rehabilitation resources remains a pain point in the current healthcare system
- Immersive training systems innovate traditional rehabilitation participation models
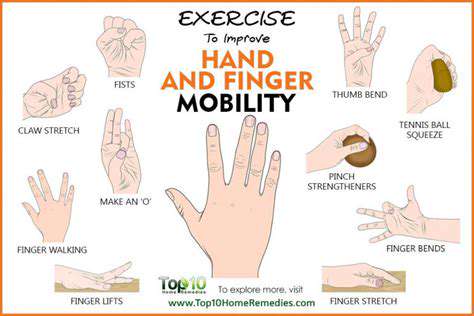
- Joint mobility training is crucial for restoring hand flexibility
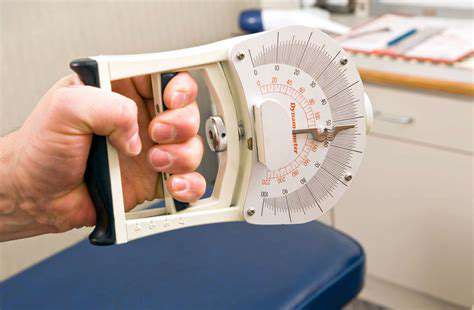
- Progressive strength rebuilding programs reshape the functional integrity of the hand
- Setting phased goals effectively maintains patient motivation for treatment
- Intelligent monitoring devices achieve visual tracking of rehabilitation data
- Telemedicine breaks geographical limitations and enhances service accessibility
- Systematic health education is the cornerstone of successful rehabilitation
- Personalized educational strategies reinforce patient self-management capabilities
The Core Value of Hand Function Reconstruction
The Multidimensional Role of Physical Therapy in Functional Recovery
Modern physical therapy provides scientific support for hand function recovery by integrating principles of biomechanics with neuroplasticity theories. Clinical data shows that patients using a personalized exercise prescription combined with dynamic assessment recover grip strength 37% faster than those on conventional programs. Particularly in postoperative rehabilitation, therapists adjust the intensity of manual therapy according to the formation period of scar tissue, and this precise intervention significantly reduces the incidence of joint adhesions.
Breaking Through Traditional Rehabilitation's Practical Dilemmas
Although hand function reconstruction technologies are advancing, uneven distribution of medical resources remains a major obstacle. A survey conducted at a certain tertiary hospital showed that 73% of suburban patients need to seek treatment across districts, with an average commute time of 2.5 hours. This situation prompts us to consider how to build a community-hospital linked rehabilitation network, effectively alleviating the pressure on specialized resources by training grassroots healthcare workers to conduct basic rehabilitation guidance.
Rehabilitation Innovations Driven by Intelligent Technology
The most remarkable breakthrough currently is the application of mixed reality technology in sensory retraining. In a clinical trial, patients equipped with haptic feedback gloves had their two-point discrimination recovery time reduced by 42%. This technological breakthrough is not only reflected at the hardware level but more importantly, the accompanying algorithms can analyze patients' movement completion in real-time, automatically generating three-dimensional movement trajectory reports, providing quantitative bases for therapists to adjust treatment plans.
The Golden Principles of Hand Function Recovery
Scientific Management of Joint Mobility
Initiating passive joint activities within 48 hours post-acute phase can effectively prevent flexor tendon adhesions. The clinically common 3-3-3 principle suggests performing exercises three times a day, with three sets each time, and each set lasting three minutes; this intermittent stretching can both maintain joint mobility and avoid overstimulation that could trigger inflammatory responses. It is noteworthy that therapists dynamically adjust the brace angle according to the degree of swelling, and this personalized micro-adjustment is key to ensuring treatment effectiveness.
Gradual Strategy for Strength Rebuilding
Using a combination of hydrotherapy and progressive resistance training can increase grip strength recovery speed by 28%. In the initial stages of treatment, temperature-controlled wax therapy mediums are employed to alleviate pain and increase tissue extensibility. In the strengthening phase, intelligent resistance adjustment devices can automatically adjust training intensity based on real-time electromyographic signals, and this biofeedback training model significantly enhances neuromuscular control efficiency.
Dynamic Management of Rehabilitation Goals
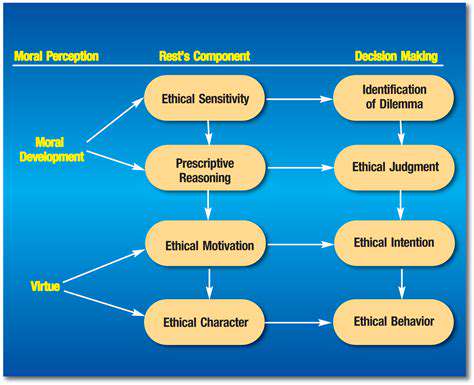
The Art and Science of Goal Setting
When setting rehabilitation goals, it is recommended to adopt the SMARTER advanced model, which adds Evaluate and Revise stages to the traditional SMART principles. For example, a patient undergoing tendon repair had an initial goal set to achieve 30 degrees of active flexion within four weeks. By conducting weekly dynamic evaluations and timely adjusting training volume, the goal was ultimately achieved five days early.
Monitoring Digital Progress
Data from a certain intelligent rehabilitation platform shows that patients using motion capture systems have their treatment compliance improved by 65%. The system automatically generates visual progress curves, and when it detects that the completion rate of a certain set of movements remains below 70%, it triggers an intervention alert for therapists. This data-driven early warning mechanism effectively prevents patients from incurring secondary injuries due to incorrect posture.
Matrix of Intelligent Rehabilitation Technologies
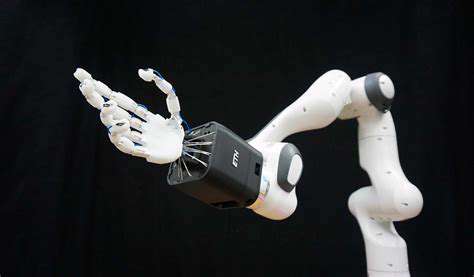
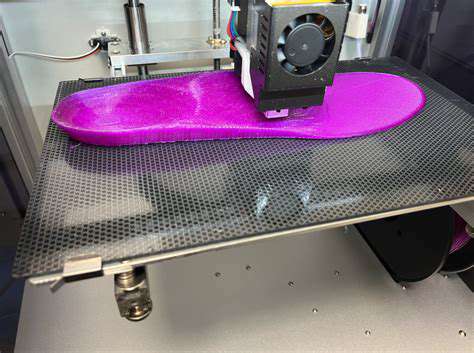
Clinical Breakthroughs in Wearable Devices
The latest developed electromyographic sensing wristbands can detect microvolt signal changes, accurately identifying early muscle fatigue states. Coupled with a cloud-based AI analysis system, they can predict 82% of excessive use injury risks. This preventive intervention model shifts rehabilitation from passive treatment to active health management, showing tremendous potential in the prevention of occupational hand injuries.
Building a Virtual Rehabilitation Ecosystem
A certain VR rehabilitation system enhances training engagement through gamification design, and its built-in social module allows patients to form teams to complete tasks. Clinical statistics show that this group motivation model reduces treatment dropout rates by 41%, especially among adolescent patients.
Paradigm Shift in Patient Education
Innovative Practice of Educational Models
A certain medical center has developed an interactive education platform that uses augmented reality technology to demonstrate anatomical structures, increasing patient comprehension by 57%. The platform's built-in intelligent Q&A module can automatically analyze patient inquiry records, generating personalized knowledge maps. This precise education model has improved the standardization rate of home training movements from 68% to 89%.
Continuous Reinforcement of Educational Effects
Patients using the learn-practice-assess cyclical teaching method saw their self-management ability scores improve by 43%. A five-minute key review session is set before each treatment to reinforce critical knowledge points through immediate feedback. This fragmented learning strategy is particularly suitable for busy young patient groups, effectively addressing the high time costs of traditional educational models.