Exploring the Benefits of Cold Therapy for Arm Injuries
The Science Behind Cold Therapy's Effectiveness
The Mechanisms of Action
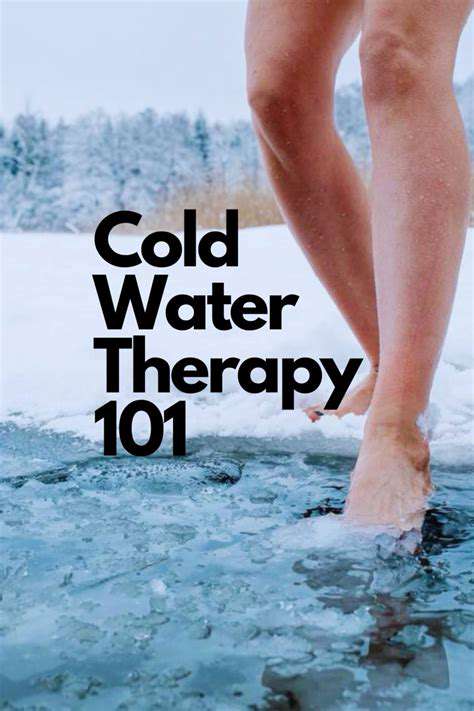
Cold therapy, encompassing various modalities like ice baths, cold packs, and cryotherapy, works by constricting blood vessels and reducing blood flow to the treated area. This immediate effect helps to minimize inflammation and reduce pain signals transmitted to the central nervous system. The principle of vasoconstriction is crucial in managing acute injuries and post-exercise soreness.
Beyond the immediate response, cold therapy can also influence the body's inflammatory cascade. By slowing down the inflammatory response, cold therapy may help to limit tissue damage and promote faster healing. This is particularly important in situations where inflammation is a significant contributing factor to pain.
Impact on Inflammation
Inflammation, a natural response to injury or stress, involves a complex interplay of cellular processes and chemical mediators. Cold therapy's ability to dampen this response is a key factor in its effectiveness in reducing pain and swelling. The reduced blood flow and altered cellular activity associated with cold therapy can help to decrease the production of inflammatory mediators, thereby lessening the inflammatory cascade.
While inflammation is a necessary process for healing, excessive inflammation can prolong the recovery period and lead to further tissue damage. Cold therapy's intervention can be vital in managing the intensity of the inflammatory response, enabling a smoother transition to the repair phase.
Effect on Pain Perception
Cold therapy's influence on pain perception arises from the reduction in nerve activity and the modulation of pain signals. By constricting blood vessels, cold therapy reduces the transmission of pain signals to the brain. This mechanism is particularly relevant for acute injuries and muscle strains, where pain relief is a primary objective.
Cryotherapy and Muscle Recovery
Cryotherapy, often utilized in professional sports, is a potent tool for muscle recovery. The immediate cooling effect reduces muscle spasms, soreness, and stiffness, allowing athletes to recover faster and perform at their peak. The precise mechanisms through which cryotherapy accelerates muscle recovery are still being investigated, but the reduction in inflammation and pain are key factors.
Safety Considerations and Practical Applications
While cold therapy offers numerous benefits, it's crucial to use it safely and appropriately. Applying ice directly to the skin for extended periods can lead to tissue damage. Always use a protective layer, such as a towel, and monitor the application time. Proper application techniques are essential for maximizing the therapeutic benefits while minimizing the risk of adverse effects.
The application of cold therapy can be tailored to various situations and conditions. From post-workout recovery to treating sports injuries, cold therapy finds widespread use in both professional and amateur settings. Understanding the science behind cold therapy allows for more informed and effective application.
Individual Variances and Considerations
Individual responses to cold therapy can vary. Factors such as pre-existing medical conditions, skin sensitivity, and the specific injury or condition being treated can impact how a person reacts to cold therapy. It's essential to consult with a healthcare professional before starting any new treatment regimen, including cold therapy, particularly if you have underlying health concerns.
Careful consideration of individual needs is paramount to ensure safe and effective application. This includes understanding potential contraindications and tailoring the treatment approach to the specific patient.
Minimizing Swelling and Inflammation with Cold Therapy

Understanding the Root Causes of Swelling and Inflammation
Swelling and inflammation are common responses to injury or illness, but understanding their underlying causes is crucial for effective management. Inflammation is a complex biological process triggered by various factors, ranging from infection to physical trauma. This intricate response involves the activation of immune cells and the release of inflammatory mediators, which contribute to the swelling, redness, and pain often associated with inflammation.
Identifying the specific cause, whether it's a bacterial infection, an allergic reaction, or an autoimmune disorder, is essential for tailoring treatment strategies. A thorough assessment by a healthcare professional is critical for determining the root cause and developing a personalized approach to managing the swelling and inflammation.
Lifestyle Modifications for Reducing Swelling
Several lifestyle modifications can significantly contribute to minimizing swelling and inflammation. Maintaining a healthy diet rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, can play a vital role. These nutrients can help reduce the body's inflammatory response and promote overall well-being.
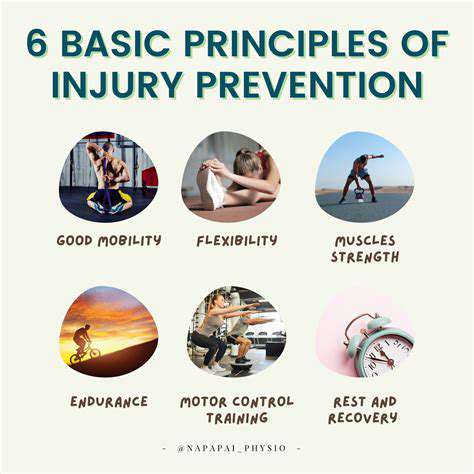
Regular exercise, including activities like walking, swimming, or yoga, can also help improve circulation and reduce swelling. Adequate hydration is equally important, as it helps flush out toxins and maintain healthy bodily functions. Proper sleep is essential for the body's natural repair processes, which can further contribute to minimizing inflammation.
The Role of Rest and Compression
Rest is crucial for allowing the body to heal and reduce inflammation. When an area is injured or inflamed, resting the affected area can significantly lessen the swelling and promote the body's natural healing processes. Proper rest also allows the body to replenish its energy reserves, which are essential for recovery and minimizing inflammation.
Applying compression, such as using elastic bandages or compression garments, can help reduce swelling by supporting the affected area and promoting lymphatic drainage. Compression helps to limit the accumulation of fluid and reduces pressure on the tissues, thus minimizing swelling and discomfort.
The Importance of Cold and Heat Therapy
Applying cold compresses to the affected area can help reduce inflammation and swelling in the initial stages following an injury or inflammation episode. Cold therapy constricts blood vessels, reducing blood flow to the area and minimizing swelling.
Heat therapy, on the other hand, can be beneficial for chronic inflammation or muscle soreness. Heat therapy increases blood flow to the area, promoting healing and reducing muscle stiffness, but should not be used in acute injury situations. Proper application of both cold and heat therapy is crucial for optimal results.
Medical Interventions and Treatments
In some cases, medical interventions may be necessary to effectively manage swelling and inflammation. Prescription medications, such as anti-inflammatory drugs, can help reduce the body's inflammatory response and alleviate pain and discomfort. These medications can be crucial in managing chronic or severe cases of inflammation.
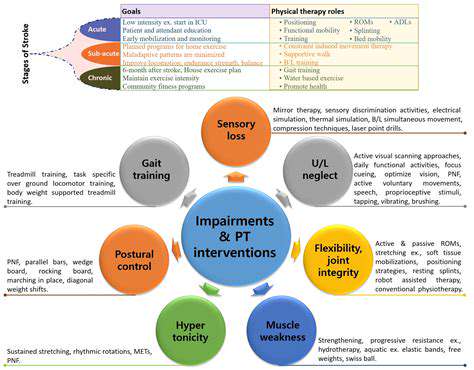
Physical therapy, occupational therapy, and other specialized treatments can also be beneficial in addressing the underlying causes of swelling and inflammation. These therapies aim to restore function, improve mobility, and promote healing.
Alternative and Complementary Therapies
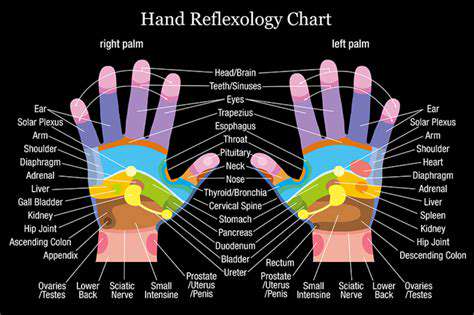
Beyond traditional medical approaches, various alternative and complementary therapies can contribute to minimizing swelling and inflammation. These include practices such as acupuncture, massage therapy, and herbal remedies.
While some research supports the efficacy of these therapies, it is crucial to consult with a healthcare professional before incorporating them into a treatment plan, especially if you are taking other medications. Always prioritize the advice of your doctor or other qualified healthcare professional regarding your specific condition and treatment needs.
Practical Application and Considerations for Cold Therapy
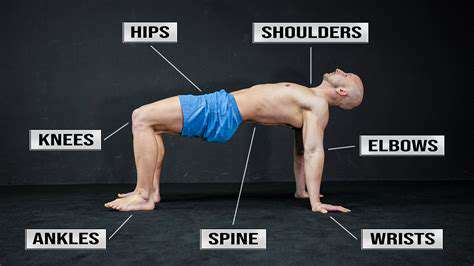
Understanding the Mechanics of Cold Therapy
Cold therapy, encompassing a range of techniques like ice baths, cold packs, and cryotherapy, works primarily by constricting blood vessels and reducing inflammation. This vasoconstriction minimizes blood flow to the affected area, thus lessening swelling, pain, and muscle spasms. Understanding this physiological response is crucial for effectively applying cold therapy and maximizing its benefits.
The localized reduction in blood flow also helps to decrease metabolic activity in the treated area. This can be particularly beneficial in the recovery phase after strenuous exercise or injury, as it helps to minimize tissue damage and promote healing.
Effective Application Techniques
Proper application of cold therapy is essential for achieving optimal results. Using ice packs directly on the skin can cause skin irritation, so wrapping the pack in a thin towel or cloth is recommended. Applying ice for extended periods (longer than 20 minutes) can be detrimental, potentially leading to frostbite. Regular breaks are crucial for preventing skin damage and ensuring the best outcome.
The duration and frequency of cold therapy sessions should be tailored to the specific needs of the individual and the nature of the injury or condition. Consulting with a healthcare professional or physical therapist can provide valuable guidance on appropriate protocols.
Cold Therapy for Muscle Soreness and Recovery
Post-workout muscle soreness, often referred to as delayed-onset muscle soreness (DOMS), is a common experience for athletes and fitness enthusiasts. Cold therapy can be a valuable tool in managing this discomfort by reducing inflammation and promoting muscle recovery. Applying ice packs or taking a cold bath following intense exercise can help to alleviate pain and hasten the recovery process.
The immediate effect of reducing swelling and pain is significant. However, the long-term benefits of incorporating cold therapy into a recovery routine extend beyond pain management, potentially improving range of motion and preventing future injuries.
Cold Therapy for Injuries and Acute Pain
Cold therapy plays a crucial role in managing acute injuries, providing rapid relief from pain and swelling. Immediately following a sprain, strain, or other acute injury, applying cold therapy can significantly reduce the inflammatory response. This immediate intervention can help prevent further tissue damage and promote a faster healing process.
By constricting blood vessels and reducing swelling, cold therapy can lessen the severity of pain associated with these injuries. This is especially valuable in the early stages of healing, where minimizing pain and swelling are crucial for effective treatment.
Considerations for Specific Conditions
While cold therapy offers numerous benefits, its application may not be suitable for all conditions. Certain individuals, particularly those with circulatory issues or compromised sensation in the affected area, should exercise caution when using cold therapy. Consulting with a physician or healthcare professional is vital to determine if cold therapy is appropriate for a specific condition.
Individuals with certain medical conditions, such as Raynaud's phenomenon, should avoid cold therapy altogether or use it with extreme caution and under medical supervision. Understanding the potential risks and contraindications is key to responsible application.
Safety Precautions and Potential Risks
Taking necessary safety precautions is paramount when using cold therapy. Care must be taken to avoid direct skin contact with the source of cold, as frostbite is a potential risk. Always wrap the cold pack in a towel or other protective material to prevent skin irritation and damage.
Furthermore, individuals with certain medical conditions, such as diabetes or peripheral neuropathy, should exercise extra caution when using cold therapy. These conditions can make individuals more susceptible to cold-related injuries. Consultation with a healthcare professional is highly recommended before incorporating cold therapy into any treatment plan.
Effectiveness and Evidence-Based Research
Numerous studies have investigated the efficacy of cold therapy in various contexts. Research consistently shows that cold therapy can be effective in reducing pain, inflammation, and swelling after injuries and exercise.
The body of evidence supporting cold therapy's effectiveness is substantial. This scientific backing underscores its value as a safe and effective treatment modality when employed responsibly and in consultation with a healthcare professional.