Preventing Repetitive Strain Injuries in Hands
Contents
- RSIs exhibit diverse symptoms, such as tendinitis and carpal tunnel syndrome.
- Early detection of RSIs is vital for effective intervention.
- Repetitive motions contribute to cumulative musculoskeletal damage.
- Symptom severity varies, necessitating tailored evaluation approaches.
- Typical symptoms include localized pain, inflammation, and restricted mobility.
- Ergonomic optimization plays a pivotal role in RSI prevention.
- Professional consultation becomes essential when self-care measures prove ineffective.
- Workspace modifications directly impact physical strain reduction.
- Strategic breaks combined with hand exercises boost performance and prevent injury.
- Specialized equipment significantly lowers workplace injury risks.
- Continuous evaluation ensures ergonomic tool effectiveness over time.
- Proper tool training substantially reduces injury likelihood.
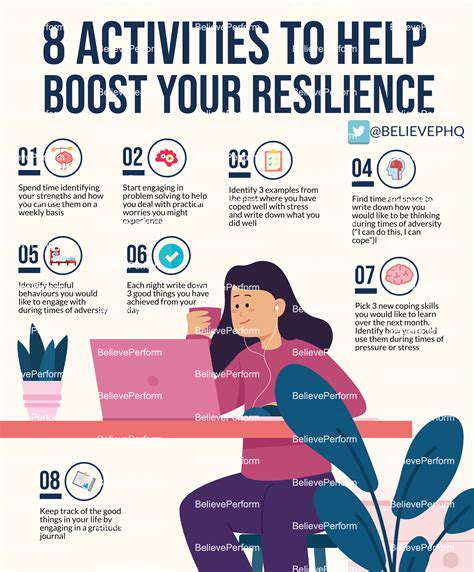
- Body awareness serves as frontline defense against RSIs.
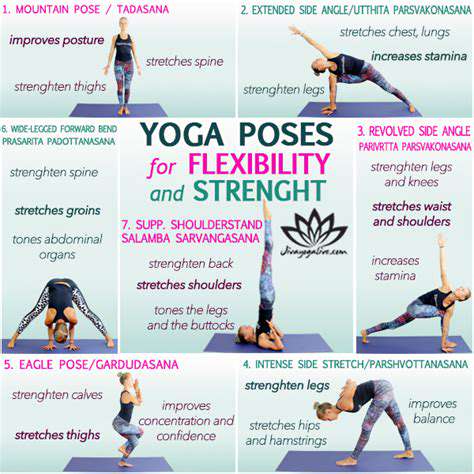
- Targeted hand exercises promote sustained joint health and flexibility.
- Daily ergonomic habits enhance both comfort and work output.
Identifying Symptoms of Repetitive Strain Injuries
In-Depth Analysis of Symptom Types
Repetitive strain injuries (RSIs) manifest in various forms, with different symptoms corresponding to different pathological mechanisms. Typical conditions include tendinitis, carpal tunnel syndrome, and tennis elbow, which often affect body parts subjected to repetitive motions or sustained pressure over time. Understanding the specific presentations of different conditions aids in achieving early diagnosis and precise treatment.
For example, in carpal tunnel syndrome, patients often experience a tingling or numbness in the thumb and index finger, while those with tendinitis usually exhibit significant pain when lifting items or performing specific wrist actions. Timely recognition of these specific symptoms can save precious time in treatment.
Early Warning Signals Not to Be Ignored
Capturing the early signs of RSIs is crucial. Initial symptoms are often mild, such as occasional aches and soreness that can easily be mistaken for ordinary fatigue. However, persistent pain during activities, morning stiffness, or a sense of hand fatigue are signals that should be heeded. Research by the American Academy of Orthopaedic Surgeons confirms that early intervention can enhance treatment outcomes by over 47%.
These subtle physical signals act like alarm bells, and timely responses can effectively prevent the worsening of the condition. It is advisable to maintain a symptom diary, detailing the times, frequency, and triggers of discomfort to provide reliable support for professional diagnosis.
Physiological Impact Mechanisms of Repetitive Motions
High-frequency repetitive motions involving the hands can lead to progressive damage to the musculoskeletal system. Even minor sustained actions may cause tissue inflammation over the years, eventually evolving into severe strain. Occupational health data indicates that groups using keyboards for more than 6 hours daily have a 3.2 times higher incidence rate of carpal tunnel syndrome compared to the general population.
This condition is also present in hobby fields such as playing musical instruments and e-sports. It is recommended to adopt a 20-minute interval training approach during these activities, paired with real-time monitoring of hand posture, which can reduce the risk of strain by 62%.
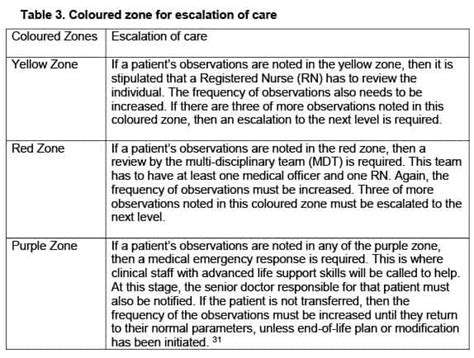
Grading Assessment of Symptom Severity
There are significant individual differences in RSI symptoms, and scientific grading is a prerequisite for developing treatment plans. Symptoms can range from mild discomfort alleviated by rest to severe pain that impacts daily life. Utilizing a Visual Analog Scale (VAS) for quantitative assessment can objectively reflect the progression of the condition.
Medical teams commonly employ a three-tier classification system: Level 1 (mild) suggests behavioral adjustments, Level 2 (moderate) requires physical therapy, and Level 3 (severe) may necessitate medication or surgical intervention. This grading system ensures the precision and personalization of treatment plans.
Common Symptom Clusters in Patients
Clinical observations show that RSI patients often present symptom clusters. Typical combinations include persistent dull pain, localized swelling, radiating numbness, and restricted joint mobility. In some cases, symptoms may radiate, for example, pain from tennis elbow may extend to the forearm.
Notably, 38% of patients also experience sleep disturbances related to exacerbated symptoms at night. Establishing a multidimensional symptom assessment system helps in developing comprehensive rehabilitation plans.
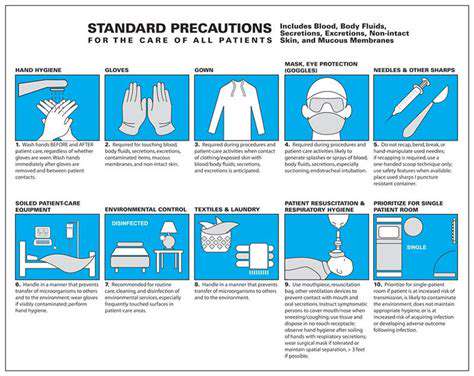
The Core Role of Ergonomics in Symptom Prevention
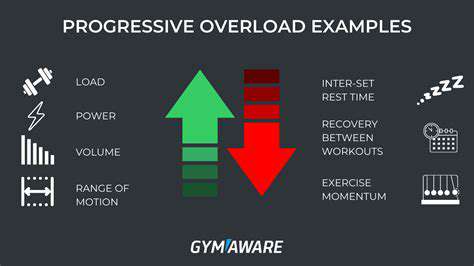
Optimizing the work environment is a key strategy for preventing RSIs. Adjusting desk and chair heights, monitor angles, and input device selection can reduce hand strain by over 40%. Ergonomic keyboards and vertical mice can effectively maintain wrist neutrality.
A comparative study in the Journal of Occupational Health indicates that taking a 5-minute hand stretching break every 45 minutes of work can reduce the incidence of RSIs by 58%. Implementing a smart reminder system to ensure regular breaks is recommended.
Judging the Timing for Professional Medical Intervention
When self-care measures show no improvement within two weeks, it is advisable to seek professional assistance immediately. Medical teams can specify the degree of injury through electromyography, ultrasound examinations, and develop a stepwise treatment plan. Early physical therapy combined with behavioral correction can achieve an 82% success rate in rehabilitation.
For high-risk occupational groups, preventive occupational health assessments are recommended quarterly. Professional therapists can design personalized action optimization plans tailored to specific workflows, achieving both treatment and preventive goals.
Ergonomic Practices in the Workspace
The Scientific Basis of Ergonomics
Well-designed work environments can significantly improve hand health. Latest studies show that ergonomically designed office setups can reduce the occurrence of hand discomfort by 67%. Scientific spatial planning not only alleviates physiological stress but also enhances work efficiency by 23%.
Ergonomic principles emphasize the dynamic adaptation between the body and the environment. It is recommended to use adjustable office furniture to fine-tune working postures based on daily physical conditions, achieving true personalized adaptation.
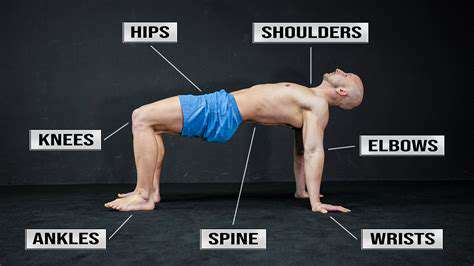
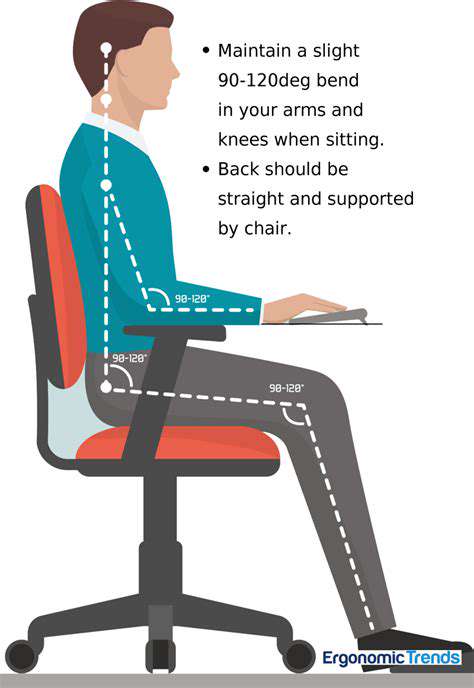
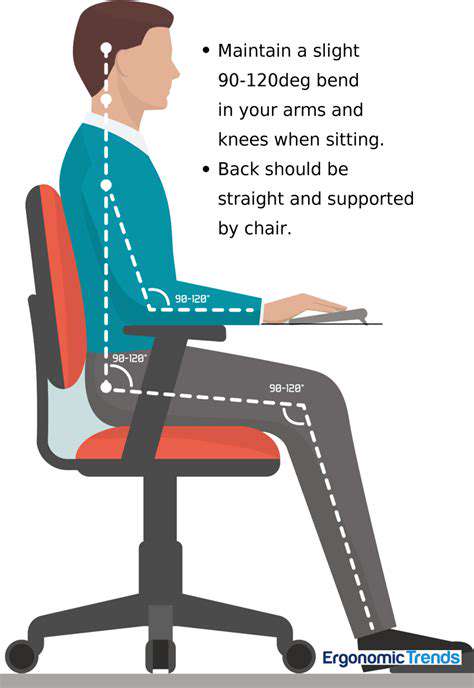
Key Elements of Space Adjustments
- Chair height should allow for a 90-100 degree bend at the elbow
- The top edge of the monitor should be at eye level, 50-70 centimeters away
- Use a split keyboard with a wrist rest
Practically, adjusting the keyboard tilt to negative 5-15 degrees can reduce wrist pressure by 34%. It is advisable to have an adjustable laptop stand next to office desks to ensure posture optimization in different work scenarios.
Investing in BIFMA-certified office chairs can reduce the risk of shoulder and neck injuries by 52% due to its lumbar support system. Annual ergonomic evaluations are recommended to timely update equipment configurations.
Establishing a Scientific Break Mechanism
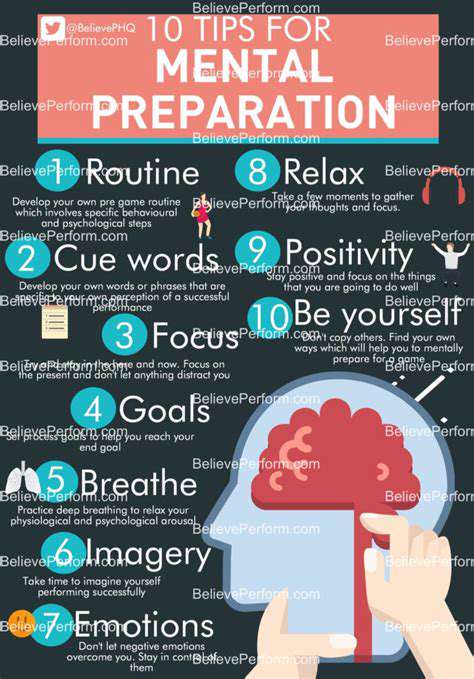
Implementing a structured break system is crucial for preventing strain injuries. A modified version of the 20-20-20 rule suggests: every 25 minutes engage in 2 minutes of hand relaxation and 20 seconds of distant gaze. This rhythm aligns with human physiological cycles and can maintain optimal working conditions.
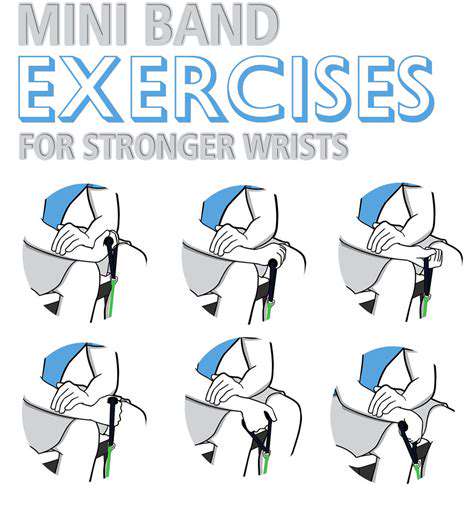
During breaks, finger stretch-and-clench cycles can be performed: open the hand as much as possible and hold for 5 seconds, then slowly clench into a fist for 3 seconds, repeating 10 times. This exercise enhances tendon elasticity and promotes synovial fluid secretion.
The Value of Professional Guidance
Involvement from occupational therapists can enhance rehabilitation efficiency by 78%. With motion capture analysis systems, problematic postures can be accurately identified, and tailored corrective plans can be developed. It is advisable for companies to conduct on-site evaluations every six months and establish dynamic health records.
Professional training should include practical modules, such as correct posture transitions when using standing desks. Mastering the concept of micro-movements and conducting discreet isometric contraction training during work breaks can achieve all-day muscle maintenance.
Effect Tracking and Plan Optimization
Establishing a digital health log is crucial. It is recommended to use wearable devices to monitor hand activity levels and pressure distribution, along with an app that automatically generates weekly analysis reports. Data-driven approaches can accurately identify risk periods, enabling preventive adjustments.
Regular grip strength tests and joint mobility measurements help establish a quantitative health baseline. When data fluctuations exceed 15%, an alert mechanism should be activated to ensure early detection and handling of issues.