Revolutionary Approaches to Wrist Pain Management
Beyond the Immediate: Addressing the Root Causes
Often, a superficial injury, like a cut or a scrape, receives immediate attention with bandages and antiseptic. However, a deeper understanding of the situation requires looking beyond the immediate visible wound. This involves acknowledging that the injury, whether physical or emotional, often stems from underlying issues. Exploring these root causes is crucial for effective and lasting healing.
Understanding the Context: Environmental and Personal Factors
The context surrounding an injury significantly impacts its healing process. Environmental factors, such as exposure to harmful elements or unsafe conditions, play a critical role. Personal factors, including pre-existing conditions, stress levels, and emotional well-being, can also influence how the body responds to an injury. Acknowledging these factors is vital for creating a supportive environment conducive to recovery.
The Importance of Prevention: Proactive Measures
Focusing solely on addressing existing injuries overlooks the critical aspect of prevention. By understanding the potential triggers or contributing factors, proactive measures can be implemented to minimize the likelihood of future injuries. This can involve implementing safety protocols, modifying behaviors, or seeking professional guidance to address underlying vulnerabilities. This approach shifts the focus from reactive repair to proactive protection.
Holistic Healing: Integrating Physical, Emotional, and Mental Well-being
True healing extends beyond the physical realm. It encompasses the intricate interplay of physical, emotional, and mental well-being. Neglecting any one of these aspects can impede the overall recovery process. A holistic approach, therefore, addresses the entire person, fostering a sense of balance and resilience. This might include therapies, stress management techniques, and support systems.
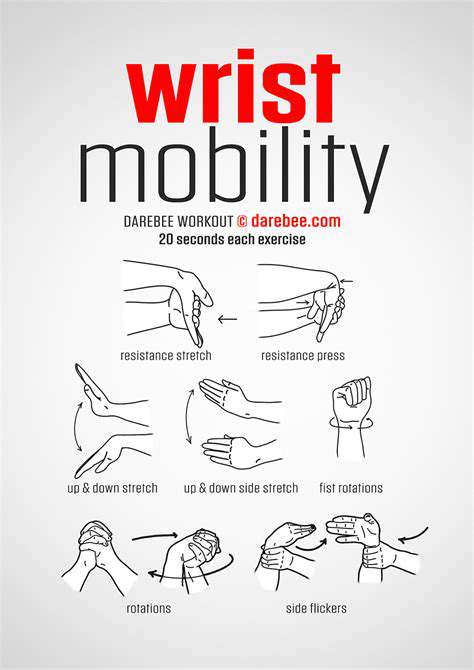
Seeking Professional Guidance: The Role of Experts
Complex injuries or prolonged recovery periods often necessitate professional guidance. Medical professionals, therapists, and counselors can provide expert advice and support, tailoring interventions to individual needs. Their expertise can illuminate hidden factors and develop personalized strategies for optimal recovery. Seeking professional help is a sign of strength, not weakness, and can significantly accelerate the healing process.
Long-Term Recovery: Building Resilience and Adaptability
Beyond the initial healing phase lies the crucial process of long-term recovery. This involves building resilience and adaptability to navigate future challenges. Developing coping mechanisms, fostering a positive mindset, and establishing healthy habits are essential for lasting well-being. These strategies are vital in helping individuals not only recover from an injury but also thrive in the face of adversity.
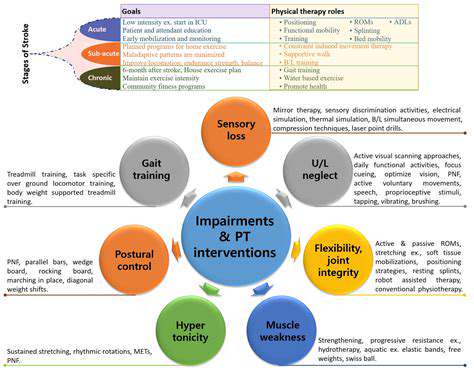
The Power of Targeted Physical Therapy: Reclaiming Wrist Function
Improving Wrist Strength and Endurance
Targeted physical therapy plays a crucial role in restoring wrist function by focusing on specific exercises that build strength and endurance. These exercises, often tailored to individual needs and limitations, progressively challenge the wrist muscles, tendons, and ligaments. This targeted approach ensures that the therapy addresses the root cause of the wrist dysfunction, preventing future injury and promoting long-term recovery. By focusing on isolated movements and gradually increasing resistance, patients can regain the ability to perform daily tasks, from simple gripping to more complex activities requiring wrist dexterity.
Exercises like wrist curls, extensions, and rotations, performed with varying resistance bands or weights, are integral components of this approach. Proper form and controlled movements are paramount to avoid exacerbating existing injuries or developing new ones. The goal is to rebuild the strength and resilience of the wrist, enabling a greater range of motion and reducing pain and discomfort associated with wrist issues. The therapist will carefully monitor progress and adjust exercises as needed, ensuring that the patient is working within their capabilities and achieving optimal results.
Restoring Wrist Flexibility and Range of Motion
A key element of targeted physical therapy for wrist issues is restoring flexibility and range of motion. This involves stretching exercises that target the muscles and tissues surrounding the wrist, improving their elasticity and reducing stiffness. These stretches are designed to gradually increase the wrist's range of motion, allowing for a more natural and pain-free movement. The therapist will guide the patient through the stretches, ensuring they are performed correctly and within a safe range to prevent further injury.
Specific stretching techniques, such as wrist flexion, extension, radial deviation, and ulnar deviation, are employed to improve flexibility. The focus on controlled stretching and gradual increases in range of motion is crucial to prevent injury and promote optimal recovery. Regular stretching sessions, combined with other physical therapy interventions, can significantly improve the overall function and mobility of the wrist, allowing patients to participate in activities they enjoy without pain or limitations.
Additionally, modalities such as heat and ice therapy may be incorporated to further enhance the effectiveness of these stretching exercises. This combined approach, focusing on both strength and flexibility, is essential for achieving a complete recovery and enabling patients to regain their full wrist function.
This targeted approach is tailored to the individual needs of each patient and may also involve the use of assistive devices or splints to support the wrist during recovery. The combination of exercise, stretching, and other therapeutic modalities creates a comprehensive plan to restore optimal wrist function.
Exploring the Potential of Platelet-Rich Plasma (PRP) Therapy
Platelet-Rich Plasma (PRP) Therapy: A Deeper Dive
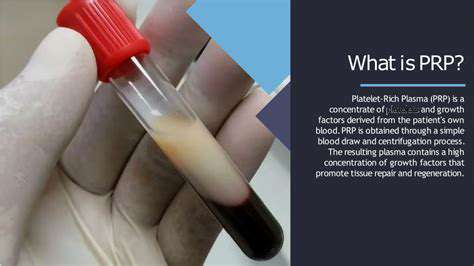
Platelet-rich plasma (PRP) therapy utilizes a patient's own blood to stimulate healing and regeneration. This innovative approach harnesses the body's natural healing mechanisms, leveraging the concentrated platelets within the plasma to accelerate tissue repair. PRP therapy has shown promise in various applications, including musculoskeletal injuries and skin rejuvenation.
The process involves drawing blood from the patient, separating the platelets from other blood components, and then concentrating the platelets in a plasma solution. This concentrated solution is then injected into the target area, where the platelets release growth factors that promote cell growth and tissue repair.
Mechanism of Action: Unveiling the Science
The potent effect of PRP therapy stems from the rich supply of growth factors contained within platelets. These growth factors, such as platelet-derived growth factor (PDGF) and transforming growth factor-beta (TGF-β), play crucial roles in the body's natural healing process. They stimulate cell proliferation, angiogenesis (the formation of new blood vessels), and collagen synthesis, all essential components of tissue regeneration.
By concentrating these vital factors, PRP therapy can effectively jumpstart the body's natural repair mechanisms, leading to faster healing and improved tissue function. Understanding the complex interplay of these growth factors is key to appreciating the therapeutic potential of PRP.
Applications Across Diverse Fields
PRP therapy finds applications in a range of medical specialties. From orthopedics, where it's used to treat musculoskeletal injuries and accelerate recovery from surgeries, to dermatology, where it's employed for skin rejuvenation and hair restoration, the versatility of PRP is remarkable. Its ability to stimulate collagen production and reduce inflammation makes it a compelling option for addressing a broad spectrum of health concerns.
Furthermore, dental procedures, sports medicine, and even veterinary medicine are exploring the potential of PRP for therapeutic purposes. The adaptability of this approach to various applications is a testament to its promising future.
Safety and Considerations for PRP Therapy
While generally considered safe, PRP therapy is not without potential risks. As with any medical procedure, complications can arise, although they are typically mild and temporary. Proper patient selection and meticulous technique are crucial for minimizing the risk of adverse events. Careful consideration must be given to individual patient factors and the specific application to ensure optimal outcomes and patient safety.
Potential side effects might include minor pain, swelling, or bruising at the injection site. Thorough evaluation and communication between the patient and healthcare provider are essential to managing any potential risks and ensuring a positive therapeutic experience.
Navigating the Landscape of Regenerative Medicine: Stem Cell Therapies
Understanding Stem Cell Therapies
Stem cell therapies represent a revolutionary frontier in regenerative medicine, offering the potential to repair damaged tissues and organs. These therapies leverage the unique ability of stem cells to differentiate into various cell types within the body. This remarkable characteristic makes them promising candidates for treating a wide range of conditions, from spinal cord injuries to heart disease, and holds the key to addressing previously incurable ailments. The journey of understanding stem cell therapies is still ongoing, but early results are undeniably encouraging and point towards a future where these therapies could transform healthcare.
Stem cells are essentially blank slates, with the potential to become any cell type in the body. This remarkable plasticity allows them to be harnessed for a wide array of regenerative medicine applications. Researchers are actively exploring various sources of stem cells, including embryonic stem cells, induced pluripotent stem cells, and adult stem cells, each with its own unique characteristics and potential benefits. The careful selection of stem cell sources is critical to ensure safety and efficacy in clinical applications. Further research and development are crucial to refine these techniques and address the ethical considerations associated with using embryonic stem cells.
The Role of Regenerative Medicine in Treating Disease
Regenerative medicine, encompassing stem cell therapies and other techniques, is poised to revolutionize the treatment of a multitude of diseases. Currently, many patients face limitations due to the inability of damaged tissues and organs to repair themselves. Stem cell therapies offer a potential solution by providing the building blocks for tissue regeneration. From repairing damaged nerve tissue after spinal cord injury to potentially restoring heart function following a heart attack, the applications are vast and hold great promise for improving the quality of life for millions.
The transformative potential of regenerative medicine extends beyond acute injuries. Chronic conditions like osteoarthritis, Parkinson's disease, and type 1 diabetes also show promise for treatment through regenerative strategies. In osteoarthritis, for example, stem cell therapies could potentially regenerate damaged cartilage, alleviating pain and restoring joint function. This burgeoning field offers hope for a future where patients with a variety of debilitating conditions can experience significant improvements in their health and well-being. The ongoing research and development in regenerative medicine are paving the way for a new era of personalized and effective treatments.
Ethical Considerations and Challenges in Stem Cell Research
While the potential of stem cell therapies is immense, ethical considerations surrounding the use of embryonic stem cells remain a significant challenge. The sourcing of these cells raises important questions about the balance between scientific advancement and ethical principles. Careful consideration of the ethical implications is crucial for ensuring that research and clinical applications are conducted responsibly and with due regard for the well-being of all stakeholders. The development of alternative cell sources, such as induced pluripotent stem cells, offers a potentially more ethically sound approach while preserving the benefits of stem cell therapies.
Beyond ethical concerns, significant scientific challenges remain. Ensuring the safety and efficacy of stem cell therapies requires rigorous testing and validation. Factors such as controlling the differentiation of stem cells into the desired cell types and preventing the formation of tumors are crucial aspects of this process. Furthermore, the development of efficient and cost-effective methods for large-scale production of stem cells is essential for widespread clinical application. Addressing these challenges will be critical for realizing the full potential of stem cell therapies and bringing them to the forefront of healthcare practices.
Future Directions and Advancements in the Field
The future of regenerative medicine and stem cell therapies looks promising, with ongoing advancements pushing the boundaries of what's possible. New techniques for delivering stem cells to target tissues and improving their survival rates are constantly being developed. Advancements in 3D bioprinting and tissue engineering are further enhancing the possibilities for regenerating complex tissues and organs. These technologies hold the potential to create functional replacements for damaged or diseased tissues, offering a transformative approach to treating a wide range of conditions.
Personalized medicine approaches are also emerging, with researchers exploring the potential of tailoring stem cell therapies to individual patient needs. This personalized approach could lead to more effective and less risky treatments, improving patient outcomes and minimizing side effects. The convergence of stem cell biology with other fields, such as nanotechnology and biomaterials, promises further breakthroughs in regenerative medicine, paving the way for a future where damaged tissues and organs can be effectively repaired and replaced, leading to a healthier and more vibrant population.