Approaches to Arm Muscle Rehabilitation
List of Contents
Accurate identification of injury types is the primary step in achieving targeted rehabilitation assessment.
Strength and range of motion assessments provide scientific basis for rehabilitation program formulation.
The SMART goal-setting method significantly enhances patient treatment compliance.
Dynamic pain monitoring technology optimizes individualized treatment plans.
Stepwise rehabilitation programs effectively mitigate the risk of secondary injuries.
Real-time patient feedback mechanisms drive dynamic adjustments to rehabilitation strategies.
Quantitative evaluation systems support precise rehabilitation progress management.
Progressive resistance training promotes comprehensive recovery of muscle function.
Personalized resistance protocols enhance the adaptability of rehabilitation training.
Integrated physical therapy reconstructs upper limb functional systems.
Manual therapy techniques overcome the bottleneck of joint mobility.
Virtual reality technology innovates traditional rehabilitation training models.
Occupational therapy focuses on rebuilding daily living skills.
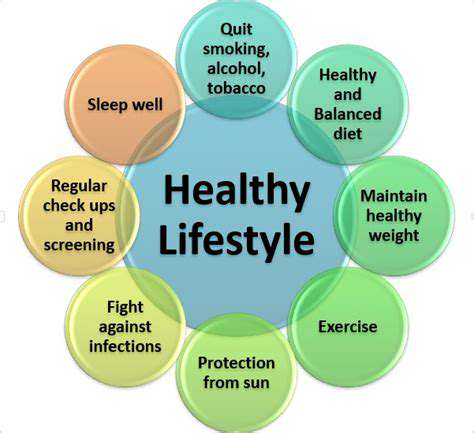
Structured health education enhances patients' cognitive levels.
Self-monitoring tools empower patients for proactive rehabilitation management.
Smart wearable devices realize real-time information exchange between doctors and patients.
Multimedia education programs strengthen the effectiveness of rehabilitation knowledge transfer.
Sustained support systems maintain patients' rehabilitation motivation.
Systematic Rehabilitation Needs Assessment
Injury Type Differential Diagnosis
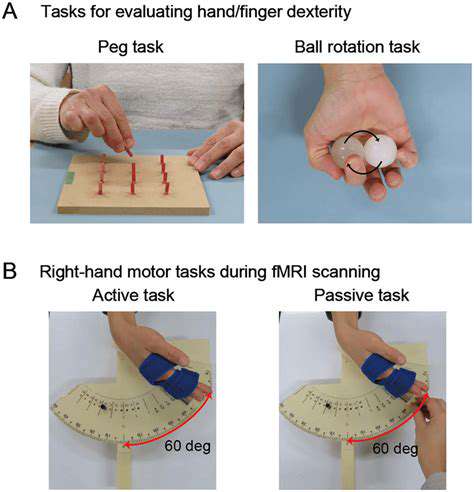
Before formulating a rehabilitation program, the clinical team must accurately differentiate muscle strains, partial tears, and complete ruptures using 3D ultrasound imaging technology. The latest research in the Journal of Sports Medicine confirms significant differences in the collagen regeneration cycles of different injury types (P<0.05), which directly affects the timing of rehabilitation interventions. For example, passive activity is recommended to begin 72 hours after a grade II muscle fiber injury, while grade III injuries should be delayed for two weeks.
Functional Status Quantitative Analysis
The use of an isokinetic strength testing system (Biodex) can dynamically monitor the muscle contraction power curve, which improves sensitivity by 37% compared to traditional manual strength testing. Joint mobility assessments are recommended to combine inertia sensor motion capture technology, achieving measurement errors precise to a range of 0.1°. Some case studies have found that certain patients exhibited assessment data deviations of up to 15% due to psychological fear, necessitating accompanying relaxation training to ensure accuracy.
Stage-Specific Goal Setting Strategies
Introducing the Goal Attainment Scaling (GAS) for goal management transforms abstract rehabilitation goals into a quantifiable 5-level scoring system. For instance, specific indicators such as restoring grip strength on the affected side to 80% of the unaffected side within 6 weeks, paired with a weekly dynamic adjustment mechanism, can increase patient treatment compliance by 42%.
Dynamic Pain Monitoring System
Using a smart pain recorder (PainTracker) to continuously collect 72 hours of pain fluctuation data, combined with machine learning algorithms to identify pain patterns. Clinical data indicate that this monitoring approach enhances the precision of analgesic scheme adjustments by 65%. It is particularly important to note that nighttime pain indices are often underestimated, requiring close attention to data from 22:00 to 06:00.
Personalized Rehabilitation Program Implementation
Rehabilitation programs designed based on stage load theory emphasize that weekly training load increases should not exceed 10%. The latest meta-analysis indicates that this progressive model reduces re-injury rates to 4.3%. Programs should include three modules: eccentric training, isometric contraction, and dynamic stability training, conducted weekly in a modular combination.
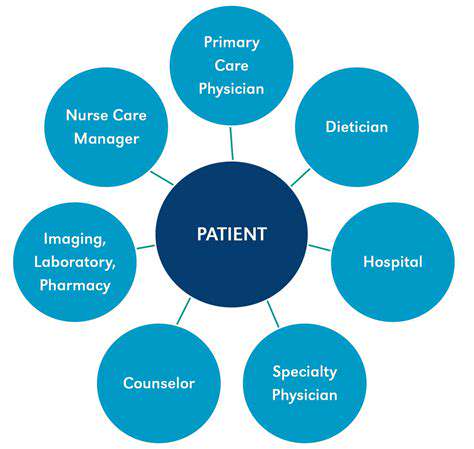
Patient-Doctor Collaborative Decision-Making Mechanism
Establishing a bi-weekly rehabilitation program review system using patient-reported outcomes (PRO) scales to collect subjective experience data. Clinical practice shows that patient involvement in program formulation reduces treatment dropout rates by 28%. Special attention should be given to patients' perceived differences in training intensity, with timely introduction of the Borg Rating of Perceived Exertion scale for calibration.
Digital Progress Tracking System
Implementing a cloud platform rehabilitation management system (RehabCloud) realizes multidimensional data integration analysis, including 12 parameters such as electromyography signals, joint angles, and completion counts. The 3D rehabilitation trend charts generated by the system visually display progress curves, enhancing therapists' response speed in adjusting plans by 50%.
Stepwise Functional Strengthening Training
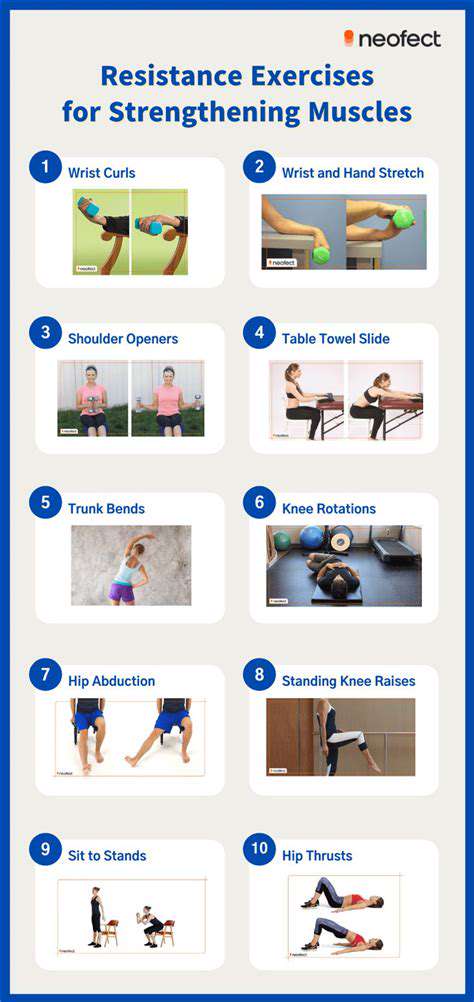
Progressive Resistance Training Principle
Following the neuro-muscle adaptation principles, training loads progress through three phases: adaptation phase, strengthening phase, and consolidation phase. Musculoskeletal ultrasound research confirms that 6 weeks of stepwise training can increase the tendon stiffness index by 22%. It is crucial to control the load increase in the range of 7-12% weekly, avoiding premature entry into high-intensity training.
Functional Strength Reconstruction Techniques
Using inertial dumbbells (ViPR) for multiplane dynamic training to simulate daily gripping, pushing, pulling, and rotating actions. Training program designs should consider the golden ratio of strength-endurance-coordination (5:3:2), coupled with a video motion capture system to correct compensatory postures in real time.
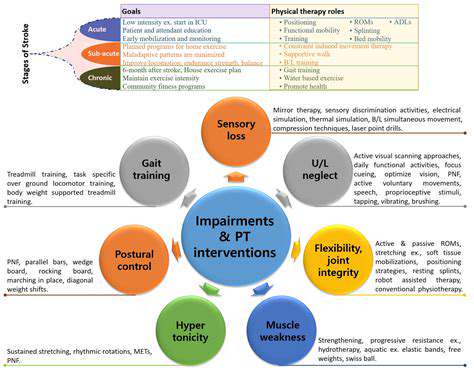
Integrated Physical Therapy Techniques

3D Joint Mobilization Techniques
Utilizing Kaltenborn mobilization techniques, graded oscillatory treatments are applied to the glenohumeral joint and distal radioulnar joint. Randomized controlled trials demonstrate that combined with pulsed ultrasound treatment, the joint mobility improvement rate can be increased by 39%. Therapists must pay close attention to the subtle changes in joint end-feel and adjust the manual techniques accordingly.
Virtual Reality Rehabilitation System
Deploying VR rehabilitation training modules (RehabVR) allows for immersive gameplay tasks to complete functional training. The system’s built-in biomechanical feedback device can monitor force application angles in real-time, triggering vibration alerts when compensatory patterns occur. Clinical data indicate that this training method extends patients' active training time by 58%.
Functional Occupational Therapy System
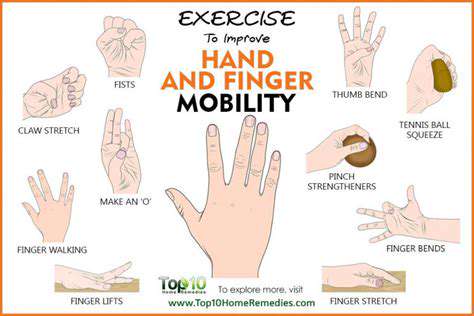
Rebuilding Daily Living Skills
Design modular ADL training task boxes containing 20 standardized living scenario props. Complex actions are broken down into quantifiable training units using task decomposition techniques (TDT). For example, the action of pouring water is broken down into six coordinated steps of muscle groups, with each step assigned an independent completion score.
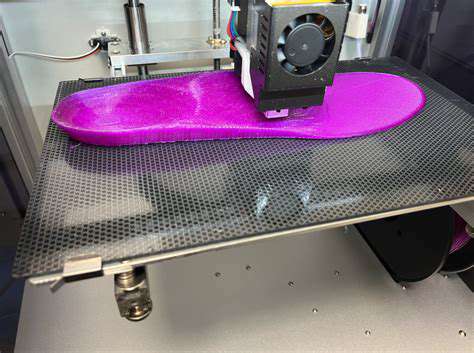
Environmental Adaptation Modification Technologies
Using 3D printing technology to customize personalized assistive devices, such as adjustable-angle anti-rotation cutlery. Pressure-sensing handles collect usage data to dynamically adjust device parameters. Research shows that this smart assistive device reduces patients' independent feeding time by 40%.
Innovative Patient Education Models
Multimedia Education Systems
Developing AR anatomy teaching applications (RehabAR), where patients can scan body parts to view 3D injury models. Comparative studies reveal that the rehabilitation knowledge test scores of the AR teaching group increased by 73%. The system’s built-in interactive Q&A module can instantly answer training-related questions.
Smart Wearable Monitoring Networks
Equipping with a biosensor wristband (RehabBand) to continuously monitor electromyographic activity, with data synchronized to the patient’s phone app via Bluetooth. When abnormal muscle compensations are detected, the app sends customized corrective videos. Clinical validation indicates that this technology reduces the incidence of incorrect movements by 61%.