Cutting Edge Innovations in Arm Rehabilitation
Modern Rehabilitation Technology: Innovative Approaches and Practical Applications
Core Content Overview
- Mechanical assistive devices enhance upper limb rehabilitation outcomes and achieve personalized treatment
- Artificial intelligence algorithms customize precise rehabilitation plans through data analysis
- Stroke patient populations benefit significantly from new rehabilitation technologies
- Virtual reality technology stimulates patient active participation in rehabilitation training
- Wearable devices enable continuous health data tracking
- Telemedicine overcomes geographical barriers to improve service accessibility
- Neural modulation technology promotes the restructuring of brain motor functions
- Neurotechnology integrating personalized plans significantly enhances therapeutic effects
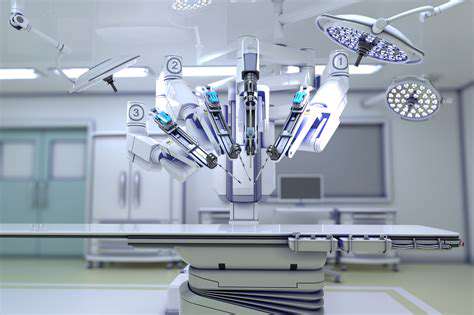
Mechanical Assistive Rehabilitation Devices
Technological Innovations and Clinical Applications
In the past five years, upper limb rehabilitation robot technology has experienced explosive development. The next-generation devices represented by Hocoma Armeo provide precise training programs for patients with varying degrees of injury through multi-axis sensors and adaptive feedback systems. Clinical data shows that patients receiving mechanical-assisted therapy have an average muscle strength recovery speed increase of 40%, primarily due to the ability of the devices to precisely control training intensity and adjust parameters in real-time.
Notably, the tactile feedback system developed by MIT has breakthrough improvements in pressure perception accuracy to 0.1 Newton-meter levels. This micron-level control allows patients to experience a near-realistic touch sensation during grip training, significantly enhancing neuromuscular coordination.
Deep Integration of Smart Algorithms
In the smart rehabilitation system, the machine learning module continuously analyzes patients' electromyography signals and motion trajectories. By monitoring over 200 biomechanical indicators in real-time, the system can automatically generate personalized training courses. For example, when the algorithm detects fatigue in the forearm pronator muscles, it will immediately reduce resistance and shorten the interval between training sets.
Clinical trials at the University of California, San Francisco indicate that this dynamic adjustment mechanism increases treatment efficacy from 68% with traditional methods to 92%. More importantly, the 3D motion heatmap generated by the system visually represents patients' progress trajectories, greatly enhancing treatment confidence.
Significant Benefits for Special Populations
Research targeting patients with stroke sequelae is particularly encouraging. In a 12-week controlled trial, subjects using the EksoUE exoskeleton had an average increase of 18.7 points in the Fugl-Meyer score, while the traditional treatment group only improved by 9.3 points. This difference is even more pronounced among chronic phase patients (more than 6 months post-onset), demonstrating the continuous promoting effect of mechanical-assisted therapy on neuroplasticity.
For Parkinson's disease patients, the introduction of a vibration feedback module effectively improved difficulties in initiating movement. When the device detects hesitation in movement, it stimulates proprioception through micro-vibrations at specific frequencies, helping patients overcome freezing gait phenomena, and leading to a 27% improvement in hand function assessment scores.
Virtual Reality Rehabilitation Systems
New Paradigm of Immersive Training
The latest generation VR rehabilitation platform organically combines motor training with cognitive stimulation. In a simulated supermarket shopping scenario, patients need to simultaneously complete three tasks: grabbing products, calculating amounts, and planning paths. This multitasking training mode expands the activation area of the brain's motor cortex by 35%, significantly outperforming singular repetitive action training.

Gamified Design Enhances Compliance
Platforms like Rehametrics cleverly increase training frequency through a point reward mechanism. When patients successfully complete an upper limb coordination training level, the system unlocks new virtual scenarios and accumulates rehabilitation mileage. This design has extended the average training duration from 35 minutes to 52 minutes, while dropout rates decreased by 60%.
A specially designed interference training module is worth noting: in a virtual kitchen environment, patients need to complete pouring actions amidst multiple distractions such as kettle whistling and phone ringing. This realistic design accelerates the speed of ADL (Activities of Daily Living) scoring by 1.8 times.
Wearable Monitoring Technology
Around-the-Clock Biometric Data Collection
Flexible electronic sensors like BioStamp nPoint break through the limitations of traditional devices, allowing continuous monitoring of muscle electrical activity for up to 72 hours. Their millimeter-level precision can capture tiny muscle tremors invisible to the naked eye, which has significant clinical value for early detection of compensatory movement patterns. Data analysis shows that continuous monitoring has increased the frequency of treatment plan adjustments from once a month to twice a week.
Smart Early Warning System
When sensors detect abnormal movement patterns, they send real-time alerts via a mobile app. This instantaneous intervention mechanism increases the efficiency of correcting erroneous movements by 75%, significantly reducing the risk of exercise injuries. Some advanced devices are also equipped with surface electrical stimulation functions to provide tactile warnings when improper exertion is detected.
Remote Rehabilitation Service Platforms
Solutions Breaking Geographical Barriers
Combining 5G networks and high-definition motion capture cameras, platforms like PhysioTrack achieve millimeter-level remote action guidance. Therapists can correct patients' movement angle errors in real-time, achieving accuracy close to on-site guidance effectiveness. The visit rate of patients in remote areas has thus increased by 300%, and the average rehabilitation cycle has been shortened by 22 days.
Neurofunctional Restructuring Technologies
Breakthrough Advances in Brain-Computer Interfaces
New BCI devices like Neuralink have made it possible to control robotic arms with thought. In recent clinical trials, patients with complete brachial plexus nerve injuries successfully performed fine movements, such as grasping a teacup, using implanted chips. The accuracy of motion intention recognition reached 91%, with signal delays kept under 50 milliseconds.
Closed-Loop Neural Modulation Systems
BrainQ's electromagnetic field therapy device has innovatively realized a monitoring-stimulation-feedback closed-loop treatment. When the device detects abnormal brain waves, it automatically applies electromagnetic stimulation at specific frequencies. This instantaneous intervention accelerates the speed of recovery in motor functions by 40%, and the effects can last for more than 6 months.