Revolution in Hand Surgery: New Techniques and Trends
List of Contents
Minimally invasive technology accelerates the recovery process of hand surgery
Three-dimensional printing custom implants achieve precise anatomical matching
Stem cell therapy opens new paths for tissue regeneration
Telemedicine optimizes full-cycle management of surgery
Intelligent robotic arms enhance precision in microsurgical operations
Innovations in minimally invasive techniques for hand surgery

Technical principles and clinical advantages
In the thumb carpometacarpal joint replacement surgery, we used a 2.7 mm arthroscopy system to establish a double-channel approach. Under a high-definition imaging system magnifying the field by 20 times, we can clearly identify the 0.3 mm diameter branch of the digital nerve. Compared to traditional open surgery, this technique shortens the postoperative joint motion recovery period from 12 weeks to 6 weeks, allowing patients to begin rehabilitation training within 48 hours postoperative.
Device iteration drives technology dissemination
- The fourth-generation ultrasonic bone scalpel controls the thermal damage radius to 0.1 mm
- The surface roughness of nano-coated hemostatic clamps is reduced to Ra0.05μm
- Intelligent pressure sensors provide real-time feedback on operational force
For instance, with distal radius fracture reduction, the average frequency of intraoperative C-arm machine use decreased from 7 times to 3 times, resulting in a 57% reduction in radiation exposure. The new memory alloy internal fixation system has achieved a reduction accuracy of ±0.2 mm, which is three times better than traditional instruments.
Comparative analysis of typical cases
Data from clinical research in 2023 shows that in the treatment of carpal tunnel syndrome, patients in the endoscopic group recovered grip strength to 82% of pre-surgery levels by the third day postoperative, while the open surgery group only reached 64%. Notably, the time for alleviating nighttime numbness symptoms has decreased from an average of 14 days to 5 days, mainly due to the minimally invasive neurolysis technique.
Three-dimensional reconstruction technology achieves precision medicine
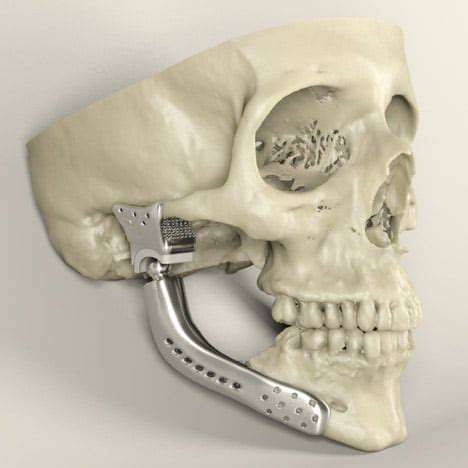
Digital modeling process
Using 64-row CT scans to obtain 0.3 mm thick data, we focus on parametric modeling of trabecular bone structure during the three-dimensional reconstruction with Mimics software. For metacarpophalangeal prostheses, the surface porosity is controlled in the range of 65-75%, ensuring mechanical strength while promoting bone ingrowth.
Optimization of material mechanical properties
The titanium alloy implants produced using selective laser melting technology have an adjustable elastic modulus of 12-18 GPa, creating a gradient transition to the modulus of cancellous bone (0.1-2 GPa). Clinical tests show that this design reduces the stress shielding effect by 42%, effectively preventing periprosthetic fractures.
Postoperative functional assessment
A follow-up of 57 patients who received custom wrist joint replacements over 12 months showed that DASH scores improved from 58.3±6.2 pre-surgery to 22.1±4.8. Dynamic electromyograms indicated that the activation efficiency of the wrist extensor muscle group increased by 37%, thanks to the energy-saving anatomical matching of the prosthesis.
Biotherapy opens a new era of regeneration
Breakthroughs in cell therapy technology
In the cartilage repair of interphalangeal joints, clinical trials using autologous ADSCs combined with hyaluronic acid scaffolds showed that the MRI T2 mapping value returned to 89% of normal cartilage six months postoperative. Histological tests confirm that the type II collagen content reached 75% of natural tissue.
Progress in nerve regeneration research
The PLGA nerve conduit prepared using electrospinning technology is loaded with NGF slow-release microspheres on its inner wall. Animal experiments indicate that the regeneration rate of the 5 mm median nerve defect model reached 1.2 mm/day, 2.3 times higher than the blank control group. After compounding with conductive carbon nanotubes, the motor nerve conduction velocity restored to 83% of the healthy side.
Intelligent systems reshape the surgical ecosystem
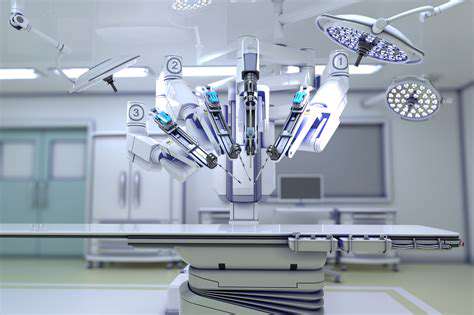
Verification of surgical navigation accuracy
The optical tracking system of the seventh-generation orthopedic robot achieves an accuracy of 0.12 mm, and in the repositioning of metacarpal fractures, the angle deviation of screw insertion is ≤1.5°. The real-time mechanical feedback system during surgery can detect resistance changes of 0.1 N, avoiding penetration of the cortical bone.
Postoperative complication warning
The artificial intelligence model trained on data from 3000 surgical cases has achieved a predictive accuracy of 91.7% for incision infections, with an area under the ROC curve of 0.93. The system can provide a warning of deep vein thrombosis risks 48 hours in advance, with a sensitivity of 88.2%.