Effective Rehabilitation Strategies for Hand Fractures
Initial Evaluation: Gathering Crucial Information
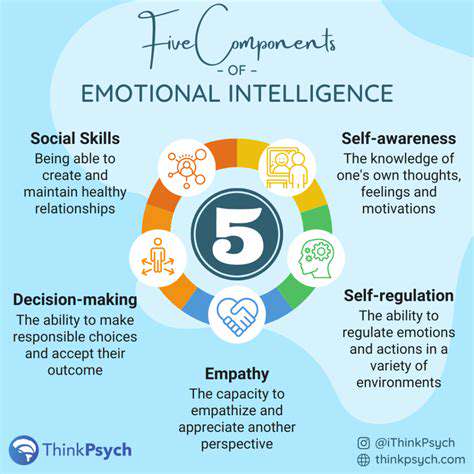
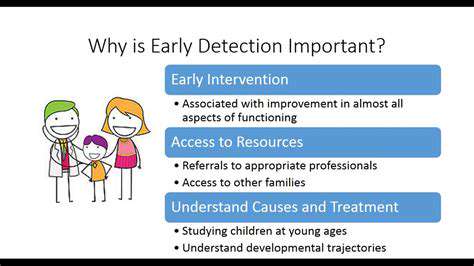
Every effective treatment plan begins with a comprehensive initial assessment. Clinicians must carefully examine not just current symptoms but also the patient's complete medical history, including past conditions and ongoing stressors. This deep dive into personal health history often reveals hidden patterns that shape treatment decisions. Reviewing existing medical records when available provides additional context that might otherwise be missed.
The evaluation process extends beyond paperwork to include hands-on physical examinations when appropriate. Various psychological assessment tools come into play - from standardized questionnaires to in-depth clinical interviews. In complex cases, neuropsychological testing can uncover subtle cognitive factors affecting treatment outcomes. This multi-pronged approach ensures no stone goes unturned in understanding the patient's unique circumstances.
Defining Treatment Goals: Establishing Clear Objectives
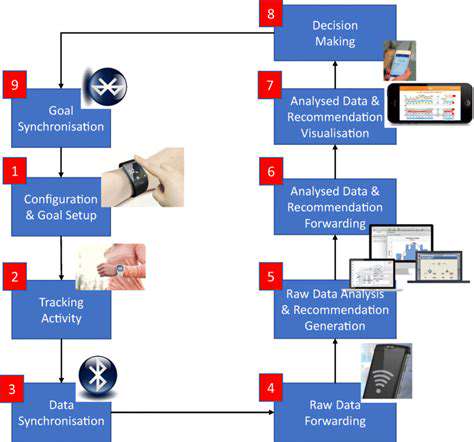
With assessment complete, the focus shifts to crafting SMART goals - specific, measurable, achievable, relevant, and time-bound targets. These objectives emerge from collaborative discussions that respect the patient's personal values and desired outcomes. When patients actively participate in goal-setting, they demonstrate significantly higher commitment to the treatment process.
Effective goals address both immediate concerns and long-term wellness. Whether reducing anxiety symptoms or developing better coping strategies, each target should contribute to sustainable improvement. Well-defined goals serve as both roadmap and measuring stick throughout treatment, allowing for timely adjustments when progress stalls or circumstances change.
Developing a Personalized Treatment Plan: Tailoring Interventions
The treatment plan translates goals into actionable steps, blending therapeutic approaches to match individual needs. This might combine individual sessions with group therapy or family counseling, depending on the situation. The most effective plans specify not just what will happen, but how often, for how long, and who's responsible for each component.
Anticipating obstacles separates adequate plans from exceptional ones. Whether addressing transportation issues, financial limitations, or scheduling conflicts, proactive problem-solving prevents avoidable setbacks. A truly personalized plan creates an environment where patients feel both supported and empowered to make lasting changes.
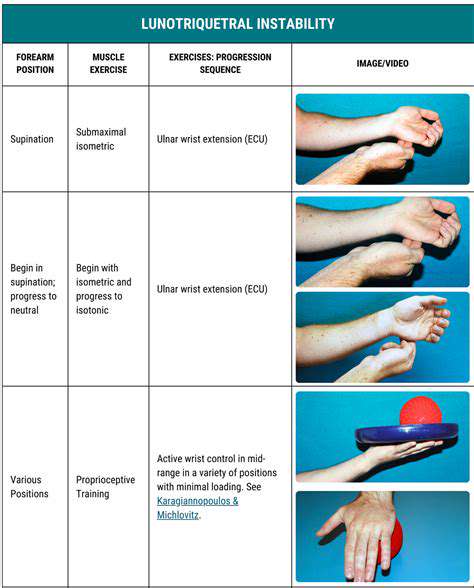
Key Principles of Hand Fracture Rehabilitation: A Multifaceted Approach

Initial Assessment and Stabilization
The first moments after a hand fracture significantly influence recovery outcomes. Clinicians must rapidly evaluate injury severity while checking for associated trauma. Precise early diagnosis prevents complications that could impair hand function permanently. Careful examination reveals telltale signs like abnormal positioning, swelling patterns, and skin integrity issues.
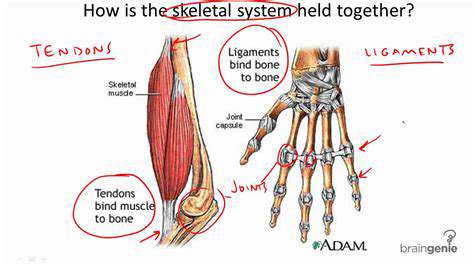
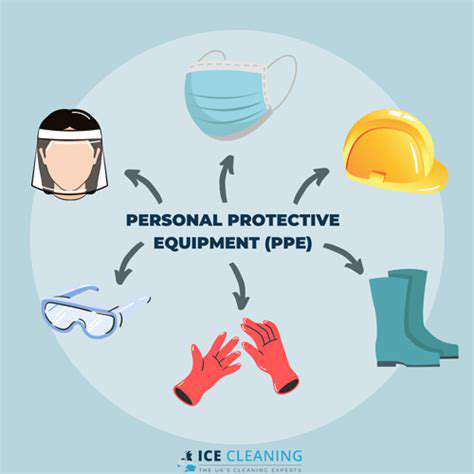
Immediate stabilization serves dual purposes - preventing further injury while establishing optimal healing conditions. Proper immobilization techniques maintain fracture alignment while allowing clinicians to better assess the injury's true nature. This critical first intervention also dramatically improves patient comfort during initial recovery.
Diagnosis and Imaging
Modern imaging technology has revolutionized fracture assessment. While X-rays remain fundamental, CT scans reveal complex spatial relationships, and MRIs expose soft tissue damage. Choosing the right imaging modality often makes the difference between adequate and exceptional treatment planning.
Radiologists look beyond obvious fracture lines to evaluate subtle displacement patterns and joint involvement. This detailed analysis directly informs whether conservative management or surgical intervention will yield better long-term results.
Treatment Options and Considerations
Treatment selection balances fracture characteristics with patient-specific factors. While stable fractures often heal well with casting, complex cases may require surgical precision. Modern fixation techniques allow even severely displaced fractures to regain near-normal function when addressed promptly.
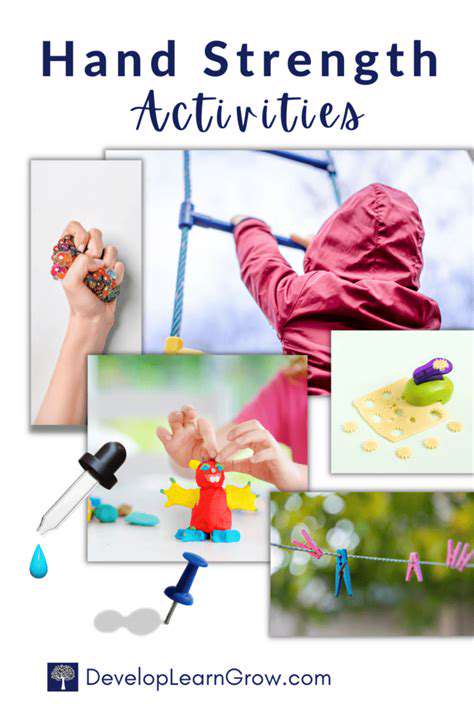
Recovery isn't passive - it requires active participation through pain management and targeted therapy. Early controlled movement prevents stiffness while promoting circulation essential for bone healing. Patient education ensures understanding of both limitations and necessary exercises during each recovery phase.
Post-operative Care and Rehabilitation
Surgical success depends equally on operative skill and post-operative vigilance. Monitoring for infection signs and proper wound care prevent most complications. Regular follow-ups allow timely intervention if healing deviates from expected patterns.
Rehabilitation transforms healed bone into functional tissue. Customized therapy programs address each patient's unique recovery challenges. Consistent effort during rehabilitation often determines whether patients regain full hand dexterity or face permanent limitations.

Financial uncertainty plagues many new ventures, but break-even analysis provides clarity. This powerful tool doesn't just predict profitability - it exposes financial vulnerabilities before they become crises. Mastery requires understanding three dynamic components: the bedrock of fixed costs, the shifting sands of variable expenses, and the oxygen of revenue generation.