Insights on Finger Tendon Repair Strategies
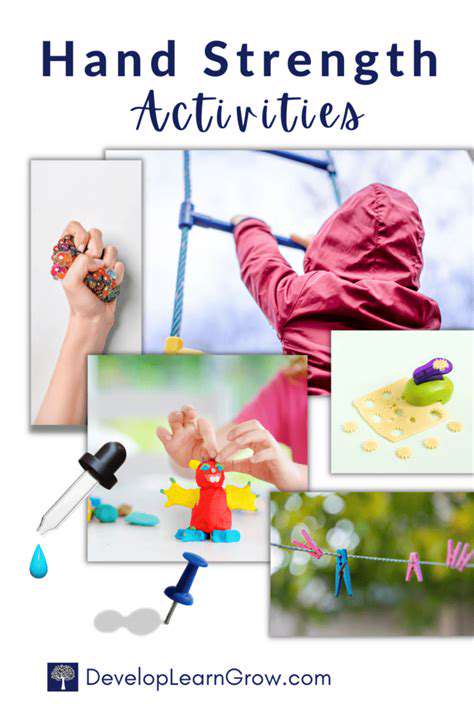
Certain activities carry disproportionate risk. Rock climbers develop unique injury patterns from sustained gripping, while boxers frequently experience rupture at the insertion points. Even mundane activities like gardening can become hazardous when improper tools force the hand into awkward positions during forceful motions. Recognizing these patterns allows for targeted preventive strategies.
Surgical Techniques for Repair
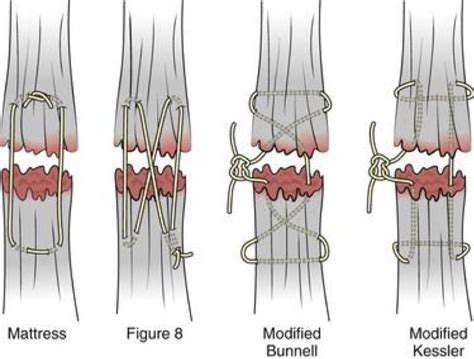
Modern tendon surgery has evolved into a precision discipline combining microsurgical skills with biomechanical understanding. The gold standard involves using specialized suture patterns that distribute tension evenly across the repair site. For complex cases, surgeons may employ tendon grafts harvested from less critical areas or synthetic reinforcement materials. The most critical technical consideration is maintaining proper tension - too loose and the repair fails, too tight and joint mobility suffers.
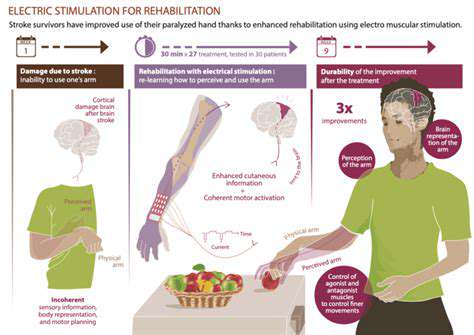
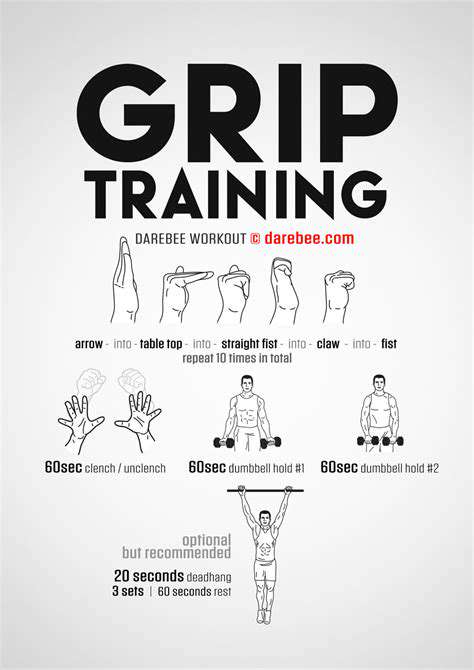
Rehabilitation protocols now begin almost immediately post-operation, a paradigm shift from traditional immobilization approaches. Early controlled motion prevents scar tissue formation while protecting the delicate repair. Advanced centers use custom dynamic splints that allow prescribed movement ranges while blocking dangerous motions. This balance between protection and mobilization represents the cornerstone of contemporary tendon recovery.
Non-Surgical Management Options
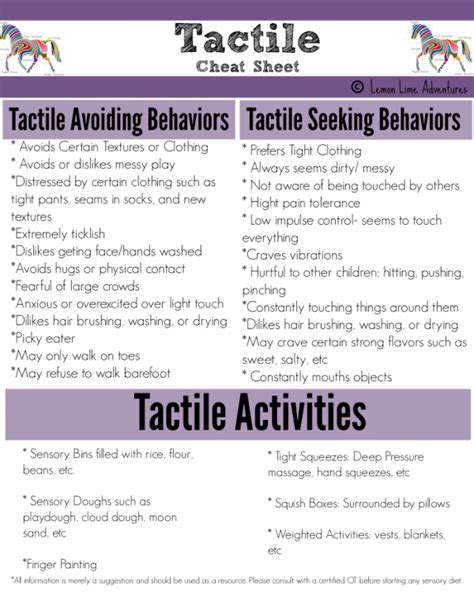
Conservative treatment plays a vital role for partial tears and less severe injuries. The cornerstone involves immobilization in carefully positioned splints that relieve tension on the damaged tendon. Recent innovations include ultrasound-guided corticosteroid injections to reduce inflammation around (not within) the tendon. Perhaps most importantly, therapists now employ tendon gliding exercises early in recovery to prevent adhesions while protecting the injury.
Emerging modalities like extracorporeal shockwave therapy show promise for stimulating healing in chronic tendinopathies. However, patient selection remains crucial - delaying necessary surgery for inappropriate conservative treatment often leads to poorer outcomes. Regular reassessment by a hand specialist ensures timely escalation to surgical options when warranted.
Surgical Techniques for Finger Tendon Repair
Minimally Invasive Techniques
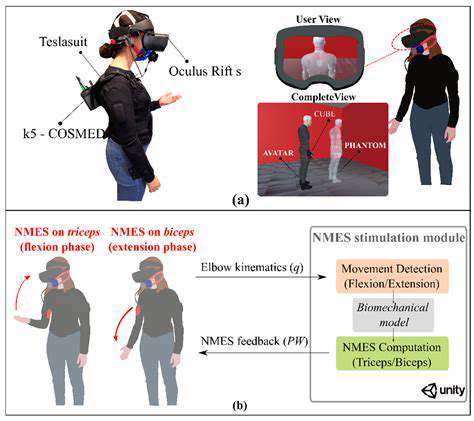
Contemporary minimally invasive approaches leverage cutting-edge technology to revolutionize tendon repair. Using specialized instrumentation through keyhole incisions, surgeons can now perform repairs that previously required extensive exposure. The real breakthrough lies in the combination of high-resolution micro cameras with instruments designed for working in confined spaces, allowing precision that rivals open techniques. Patients benefit from dramatically reduced soft tissue trauma, translating to faster functional recovery.
These techniques particularly excel in zone II flexor tendon repairs - historically the most challenging area due to the tight pulley system. By preserving these critical pulleys rather than dividing them for access, surgeons maintain the finger's intricate biomechanics. The latest generation of barbed sutures further enhances these procedures by eliminating knot bulk that could impede gliding.
Open Surgical Procedures
Traditional open surgery maintains its place for complex multi-tissue injuries requiring comprehensive reconstruction. The direct visualization allows for addressing concomitant damage to nerves, vessels, and joints that might be missed with limited approaches. In cases of delayed presentation where scar tissue has formed, the open approach provides the necessary access for meticulous scar excision and anatomical restoration.
Modern open techniques have evolved significantly from their predecessors. The use of operative microscopes and microsurgical instruments enables repairs with 8-0 or even 10-0 sutures - thinner than a human hair. For massive tissue loss, vascularized tendon transfers from the foot provide living grafts with their own blood supply, dramatically improving integration.
Post-Operative Care and Rehabilitation
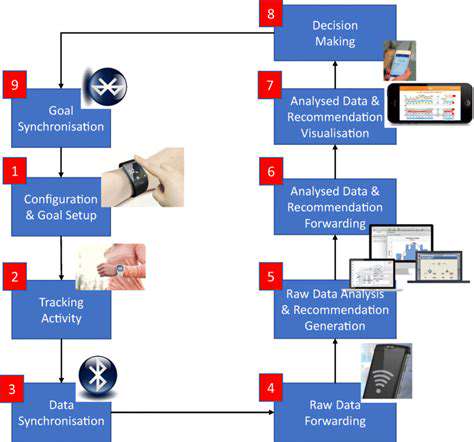
The rehabilitation journey begins in the operating room with the placement of specialized motion-friendly suture techniques. Current protocols emphasize place and hold exercises within days of surgery, a radical departure from traditional six-week immobilization. Therapists now use force-monitored systems to ensure exercises stay within safe parameters while progressively challenging the healing tissues.
Cutting-edge adjuncts include continuous passive motion devices that gently cycle the finger through prescribed ranges and biofeedback systems that help patients avoid compensatory movements. Perhaps most importantly, psychological support addresses the frustration inherent in prolonged recovery, helping patients maintain compliance during the months-long process.
Gauff's early career breakthroughs demonstrated a maturity beyond her years, with strategic adaptations that belied her limited professional experience. What set these victories apart was her uncanny ability to identify and dismantle opponents' game plans mid-match, a skill even seasoned veterans struggle to master.