Revolutionary Trends in Wrist Rehabilitation Practices
The Role of Technology in Wrist Rehabilitation: Enhanced Outcomes and Efficiency
Improving Mobility Through Assistive Devices
Modern rehabilitation has been transformed by cutting-edge assistive technologies that enhance wrist mobility during recovery. These innovative tools incorporate precision sensors and customizable settings, offering targeted support that adapts to each patient's unique needs. By providing controlled resistance and movement guidance, they enable safer, more effective exercises that accelerate healing while minimizing re-injury risks.
Clinical settings now utilize specialized splints that maintain optimal wrist positioning during healing phases. More advanced solutions include robotic exoskeletons that replicate natural wrist kinematics with millimeter precision. What sets these apart are their integrated biofeedback systems - patients receive real-time performance data, creating an interactive rehabilitation experience that promotes active participation in the recovery process.
Personalized Exercise Regimens Using AI
The integration of artificial intelligence has revolutionized how therapists develop rehabilitation protocols. Sophisticated algorithms now process multiple data points - from initial injury assessments to daily progress metrics - creating truly individualized treatment plans. This data-driven approach ensures each exercise regimen precisely matches the patient's current capabilities and recovery stage, eliminating the one-size-fits-all limitations of traditional therapy.
AI's true power emerges in its dynamic adjustment capabilities. The system continuously analyzes patient performance, automatically modifying exercise difficulty and intensity. This responsive methodology not only optimizes recovery timelines but also significantly reduces the likelihood of overexertion or therapeutic plateaus that can hinder progress.
Enhanced Visualization and Feedback Mechanisms
Digital rehabilitation platforms have transformed patient engagement through advanced motion visualization technologies. High-fidelity 3D modeling software renders wrist movements with clinical accuracy, providing immediate visual feedback on alignment, range of motion, and force application. This tangible representation of progress serves as powerful motivation, helping patients understand the direct impact of their efforts on recovery outcomes.
The psychological benefits of this visual feedback cannot be overstated. Patients report higher treatment adherence when they can literally see their improvements over time. Therapists leverage these detailed movement analytics to make micro-adjustments to treatment plans, creating a precision rehabilitation approach that was previously impossible.
Remote Monitoring for Enhanced Accessibility
Tele-rehabilitation technologies have dismantled geographical barriers to quality care. Wearable motion sensors paired with cloud-based monitoring platforms enable clinicians to track recovery metrics remotely with laboratory-grade accuracy. This paradigm shift particularly benefits rural patients and those with limited mobility, ensuring continuous access to specialist care regardless of location.
The operational efficiencies are equally transformative. Clinicians can monitor multiple patients simultaneously, intervening only when the system detects deviations from expected recovery trajectories. This optimized workflow allows therapists to focus their expertise where it's needed most while maintaining rigorous oversight of all cases.
Data-Driven Insights for Improved Treatment
Modern rehabilitation generates vast datasets that reveal previously invisible recovery patterns. By aggregating anonymized patient data, researchers can identify which interventions prove most effective for specific injury types and demographic groups. These evidence-based insights continuously refine clinical best practices, creating an ever-improving standard of care.
The longitudinal data collected enables predictive modeling of recovery trajectories. Clinicians can now anticipate potential plateaus or complications before they occur, proactively adjusting treatment plans. This shift from reactive to predictive care represents one of the most significant advancements in rehabilitation medicine.
Cost-Effectiveness and Efficiency Gains
While advanced rehabilitation technologies require initial investment, their long-term economic benefits are substantial. Digital therapy platforms reduce the need for frequent in-person visits, significantly lowering transportation costs and time commitments for patients. The precision of automated systems also shortens average recovery times, enabling faster return to productivity.
Healthcare systems benefit from optimized resource allocation. With remote monitoring handling routine progress tracking, clinical staff can focus their expertise on complex cases requiring hands-on intervention. This stratified care model maximizes both clinical outcomes and operational efficiency.
Improved Patient Outcomes Through Increased Engagement
Gamification elements in digital rehabilitation platforms have dramatically improved patient compliance. Interactive challenges, achievement milestones, and social sharing features transform mundane exercises into engaging experiences. This psychological approach to rehabilitation yields measurable improvements in adherence rates and final outcomes compared to traditional methods.
The empowerment effect is equally significant. Patients equipped with detailed performance data become active partners in their recovery rather than passive recipients of care. This shift in dynamic fosters greater accountability and motivation throughout the rehabilitation journey.
Utilizing Regenerative Therapies for Wrist Injuries: Promising New Frontiers
Harnessing the Power of Stem Cells
Stem cell research has opened unprecedented possibilities in tissue regeneration. These remarkable cells demonstrate unparalleled capacity to differentiate into specialized cell types, offering potential solutions for cartilage defects and ligament damage that traditional treatments cannot address. The field continues to evolve with improved isolation and cultivation techniques that enhance therapeutic efficacy.
Current clinical applications utilize mesenchymal stem cells harvested from bone marrow or adipose tissue. These adult stem cells avoid the ethical concerns of embryonic sources while demonstrating impressive regenerative potential. Ongoing research focuses on optimizing delivery methods and pre-treatment conditioning to maximize engraftment success rates.
Enhancing Tissue Regeneration Through Growth Factors
Cytokine therapies represent another breakthrough in regenerative medicine. Precisely timed growth factor applications can stimulate dormant repair mechanisms, accelerating natural healing processes that often remain incomplete after significant wrist trauma. Platelet-rich plasma (PRP) injections have shown particular promise in treating tendinopathies and early-stage arthritis.
The challenge lies in developing sustained-release delivery systems that maintain therapeutic concentrations at injury sites. Novel hydrogel carriers and microsphere technologies are addressing this limitation, potentially transforming growth factor therapy from intermittent injections to continuous treatment modalities.
Biomaterials for Scaffolding and Delivery
Advanced biomaterials now provide the structural framework for guided tissue regeneration. These engineered matrices replicate the mechanical and biochemical properties of native extracellular matrix, creating optimal microenvironments for cellular repopulation. Decellularized tissue scaffolds offer particularly exciting possibilities, preserving natural architecture while eliminating immunogenicity concerns.
The latest innovations include smart scaffolds embedded with biosensors that monitor regeneration progress. These responsive materials can adjust their degradation rate or release encapsulated growth factors based on real-time healing metrics, creating truly dynamic regeneration environments.
Personalized Medicine Approaches in Regenerative Therapies
The convergence of genomics and regenerative medicine enables unprecedented treatment personalization. Genetic screening now identifies patients most likely to respond to specific regenerative approaches, while biomarker analysis helps predict individual healing trajectories. This precision medicine paradigm minimizes trial-and-error in treatment selection.
Autologous cell therapies represent the ultimate in personalized medicine. By using a patient's own cells, these approaches eliminate rejection risks while capitalizing on individual healing potentials. Banking a patient's stem cells during youth for potential future use is an emerging concept that could revolutionize lifelong musculoskeletal care.
Challenges and Ethical Considerations
Despite remarkable progress, regenerative medicine faces significant hurdles. Standardization remains elusive, with treatment protocols varying widely between institutions. The high costs of many regenerative therapies also create accessibility challenges that must be addressed as technologies mature.
Ethical debates continue regarding the use of certain cell sources and genetic modification techniques. Establishing clear regulatory frameworks that balance innovation with patient safety remains an ongoing priority for the field.
Clinical Trials and Regulatory Pathways
The transition from laboratory breakthroughs to clinical applications requires rigorous validation. Multicenter trials employing standardized outcome measures are essential to demonstrate consistent efficacy across diverse patient populations. The FDA's evolving regulatory pathways for cell-based products reflect the unique challenges of these living therapies.
Post-marketing surveillance assumes particular importance in regenerative medicine. Long-term follow-up studies tracking decade-long outcomes will be crucial to fully understand the durability and potential late effects of these innovative treatments.
Future Directions and Emerging Technologies
The next frontier involves integrating multiple regenerative approaches. Combining stem cells, growth factors, and smart biomaterials in precisely engineered constructs could enable complete tissue regeneration rather than mere repair. 3D bioprinting technologies are making this vision increasingly feasible.
Gene editing tools like CRISPR may soon allow precise modification of therapeutic cells to enhance their regenerative capacities or resistance to inflammatory environments. These advancements could overcome current limitations in treating chronic degenerative conditions.
The Importance of Early Intervention and Prevention Strategies
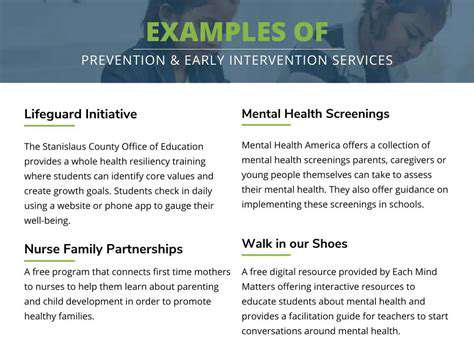
Early Detection and Intervention
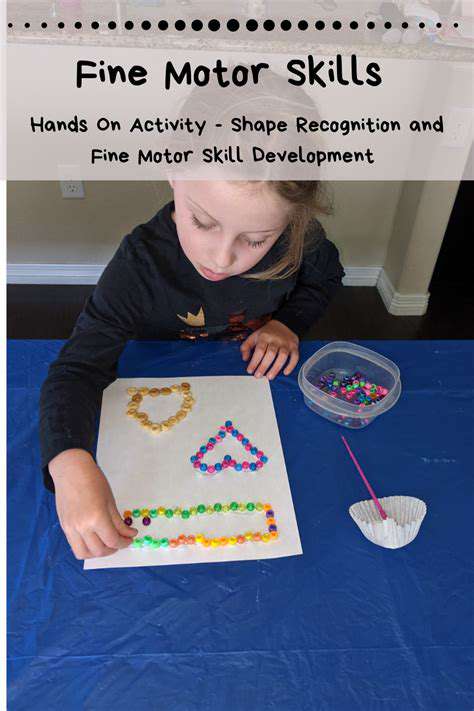
Timely identification of developmental concerns creates critical windows for effective intervention. The neuroplasticity of young nervous systems makes early childhood particularly responsive to therapeutic input. Modern screening tools can detect subtle motor or sensory differences long before they manifest as functional limitations.
Contemporary early intervention emphasizes family-centered care. Rather than isolated therapy sessions, therapists now coach caregivers in embedding therapeutic activities into daily routines. This ecological approach yields more consistent progress while empowering families as active participants in their child's development.
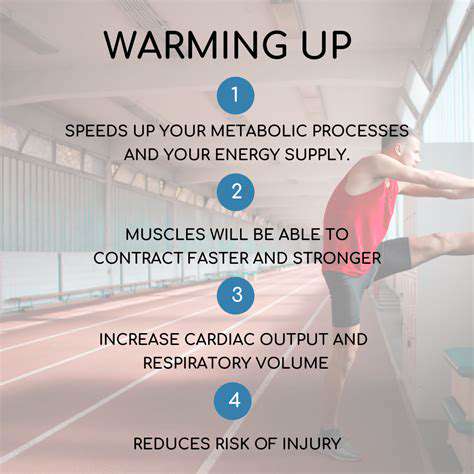
Preventive Measures for Optimal Development
Proactive strategies significantly reduce the incidence of developmental challenges. Community education programs that promote developmental milestones awareness enable earlier recognition of potential concerns. Simple environmental modifications, like ergonomic workstations for students, can prevent many musculoskeletal issues before they begin.
Nutritional interventions represent another powerful prevention tool. Ensuring adequate intake of key micronutrients during critical growth periods supports optimal neuromuscular development. Community-based cooking classes and food access programs address both nutritional and social determinants of health.
Strengthening Communities for Successful Outcomes
Effective prevention requires cross-sector collaboration. Schools, healthcare providers, and community organizations must align their efforts to create seamless support networks. Shared data systems can identify at-risk populations while protecting individual privacy.
Workplace ergonomic programs demonstrate how prevention can extend across the lifespan. By educating employers and employees about proper body mechanics and workstation setup, many repetitive strain injuries become preventable rather than inevitable.
Addressing Systemic Barriers to Early Intervention
Equitable access remains a persistent challenge. Telehealth platforms are helping bridge geographic gaps, bringing specialist expertise to underserved areas. Mobile screening units extend services directly into communities with transportation barriers.
Policy advocacy must focus on sustainable funding models. Demonstrating the long-term cost savings of early intervention helps secure necessary resources. Outcome-based reimbursement structures incentivize quality while controlling costs.