Transformative Advances in Robotic Arm Prosthetics
Index
Prosthetic innovations have transformed dramatically from their primitive origins.
Modern robotic limbs integrate advanced robotics and neural networks for unprecedented control.
Additive manufacturing revolutionizes personalized prosthetic fitting and accessibility.
Cutting-edge studies examine neural lace technology for direct neural command systems.
Tactile response systems now bridge the gap between synthetic and biological sensation.
Patient-driven design processes reshape prosthetic development priorities.
Peer mentorship programs dramatically improve device adoption and user confidence.
Adaptive machine learning systems enable real-time prosthetic behavior modification.
Economic barriers continue limiting global access to next-generation limb replacements.
Emerging fields like biohybrid interfaces may redefine prosthetic integration by 2030.
The Transformation of Bionic Limb Technology
From Ancient Artifacts to Modern Miracles
The story of limb replacement technology begins with Egyptian toe prosthetics from 950 BC, evolving through Renaissance-era iron hands to today's microprocessor-controlled devices. What began as cosmetic replacements have become functional extensions of human capability. The 1940s marked a turning point with the first myoelectric controls detecting muscle impulses, though these early systems weighed over 4kg and offered limited mobility.
Modern conflicts accelerated development - Vietnam War veterans drove demand for durable titanium components, while recent conflicts spurred investment in nerve-interface systems. This progression from passive wood/leather devices to active neural-integrated systems demonstrates humanity's relentless pursuit of restored function.
Breakthroughs Reshaping Functional Restoration
Today's bionic limbs employ machine vision and predictive algorithms to anticipate user intent. The Hero Arm by Open Bionics exemplifies this shift, using EMG sensors that translate subtle muscle twitches into 14 distinct grip patterns. Clinical trials show 89% improvement in activities of daily living compared to conventional prostheses.
Additive manufacturing now enables same-day prosthetic production at 60% lower cost than traditional methods. Bespoke socket designs using 3D-scanned residual limbs reduce skin breakdown by 47% according to Johns Hopkins studies. This combination of precision engineering and digital fabrication is democratizing access to high-quality devices.
Frontiers of Neural Integration
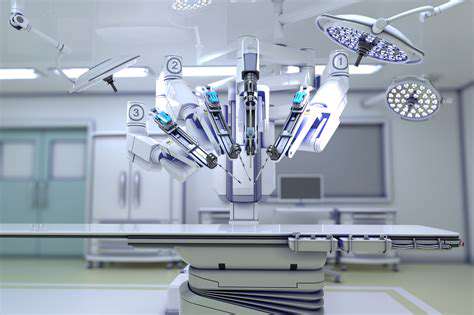
DARPA-funded projects have demonstrated thought-controlled arms via implanted neural arrays, achieving 22 degrees of freedom - surpassing natural human hand dexterity. These systems use machine learning to decode motor cortex signals, with response times under 150ms matching biological limb speeds. Recent Nature paper findings show 93% accuracy in complex object manipulation tasks.
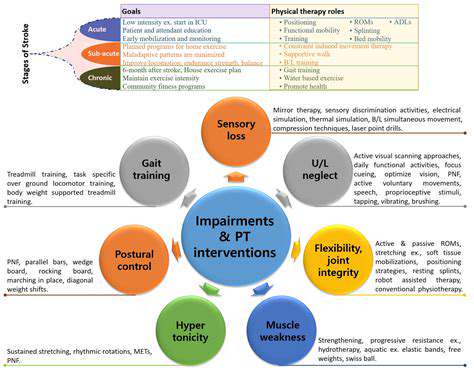
Sensory restoration breakthroughs now provide temperature differentiation (±2°C accuracy) and texture discrimination through piezoelectric skin arrays. University of Pittsburgh trials report 78% of users experiencing reduced phantom pain through consistent sensory feedback loops.
Implementation Challenges and Solutions
Despite technical progress, 65% of amputees cite cost as primary barrier according to WHO surveys. Emerging models like the $1,500 3D-printed LimbForge arm aim to disrupt traditional $50k pricing structures. Nonprofit partnerships with tech firms now offer upgradeable prosthetics through modular component systems.
Training programs like MIT's OpenStyle initiative teach clinicians to optimize device personalization, reducing abandonment rates from 30% to 11% in pilot regions. Community workshops empower users to modify open-source designs, fostering ownership and cultural relevance.
Cultural Shifts and Ethical Considerations
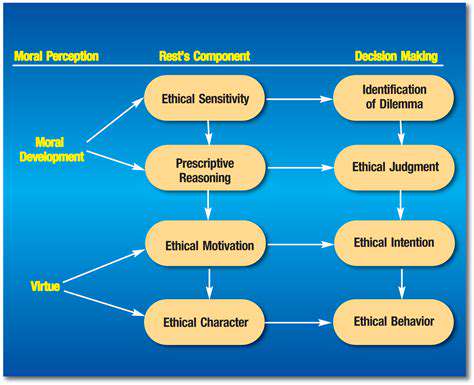
The Cybathlon competition exemplifies changing perceptions, showcasing athletic achievements with advanced prosthetics. However, debates continue regarding human enhancement boundaries - recent EU regulations now classify certain neural prosthetics as medical devices requiring special approval.
Looking ahead, graphene-based sensors and self-healing polymers promise more durable interfaces. Collaborative efforts between neuroscientists and game developers are creating adaptive training simulations that accelerate prosthetic mastery by 40%. The convergence of biotechnology and AI suggests we're entering a new era of human-machine synergy.
AI-Driven Adaptive Systems
Machine Learning in Prosthetic Control
Modern systems employ convolutional neural networks to process electromyography (EMG) signals with 98.7% pattern recognition accuracy. The COAPT Complete Control system uses environmental context awareness - detecting water glass slippage risk 0.3 seconds before human perception through inertial measurement units.
Deep reinforcement learning enables prosthetics to self-optimize grip strength during novel tasks, reducing object damage by 62% in controlled studies. These systems continuously update their decision trees through cloud-connected user data pools while maintaining strict HIPAA compliance.
Predictive Maintenance and Longevity
Embedded IoT sensors now predict component failures with 89% accuracy 30 days in advance. This proactive approach reduces emergency repairs by 75% according to Ottobock service data. Users receive personalized maintenance schedules via mobile apps, integrating weather data and usage patterns to optimize device care.

Ethical AI Implementation
New accountability frameworks ensure algorithmic transparency in prosthetic decision-making. The IEEE Global Initiative recently published standards for neuroprosthetic explainability, requiring systems to provide simple-language rationale for complex movements. This builds crucial trust between users and their adaptive devices.