Approaches for Managing Finger Tendonitis
Conservative Management: Non-Surgical Approaches to Relief

Conservative Management Approaches
When dealing with musculoskeletal or soft tissue injuries, doctors often recommend non-surgical treatments first. These methods focus on reducing discomfort while helping the body heal naturally. What makes this approach effective is its personalized nature - treatments are carefully adjusted for each person's unique situation. The process typically combines different therapies with practical lifestyle changes.
Before starting any treatment, healthcare providers conduct thorough evaluations. They use physical exams, imaging tests, and sometimes lab work to pinpoint the exact problem. Getting the diagnosis right is absolutely essential for creating a treatment plan that actually works.
Physical Therapy and Rehabilitation
Movement-based therapies form a cornerstone of non-surgical treatment. Therapists design specific exercises to rebuild strength and flexibility in affected areas. Treatment might include hands-on techniques, specialized equipment like therapeutic ultrasound, or carefully monitored exercise routines. These sessions are always supervised by licensed professionals.
The road to recovery requires consistent effort with prescribed exercises. A well-structured rehab program helps patients safely regain their abilities while preventing new injuries. Success depends on sticking to the plan and gradually increasing activity levels under professional guidance.
Medications and Pain Management
Doctors often prescribe medications to control inflammation and discomfort during healing. Options range from common anti-inflammatory drugs to specialized pain relievers. Proper pain control isn't just about comfort - it allows the body to heal more effectively. Medical professionals carefully consider each patient's health history when recommending medications.
Monitoring medication effects is crucial. Doctors adjust dosages as needed and educate patients about possible side effects to watch for during treatment.
Lifestyle Modifications and Dietary Changes
Healing isn't just about treatments - daily habits matter too. Patients receive advice on activity adjustments, rest periods, and maintaining healthy body weight. Simple changes in daily routines can dramatically impact recovery speed and long-term results. Nutrition also plays a key role, with specific dietary recommendations to support tissue repair.
Dietary adjustments might include increasing protein intake or adding anti-inflammatory foods. These nutritional changes work best when combined with other treatment elements for comprehensive healing support.
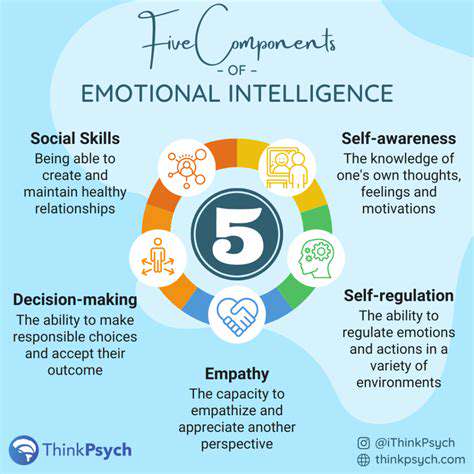
Patient Education and Self-Management
Understanding their condition helps patients become active participants in recovery. Healthcare providers explain what to expect, how to follow treatment plans, and warning signs to watch for. When patients truly understand their situation, they're much more likely to stick with treatments and achieve better outcomes. This knowledge also helps prevent future problems.
Good education covers all aspects - from the nature of the condition to practical self-care techniques and realistic recovery expectations.
Surveillance and Follow-up Care
Regular check-ins allow doctors to track progress and adjust treatments as needed. This ongoing monitoring catches potential complications early and ensures treatments remain effective. Follow-up visits are essential for evaluating whether non-surgical approaches are working or if alternatives should be considered.
During follow-ups, healthcare providers assess how patients respond to treatment and make necessary modifications. This proactive approach helps patients navigate their recovery journey with appropriate support at every stage.
The Role of Splinting and Bracing: Supporting Your Fingers During Healing
Splinting for Fracture Stabilization
Splints serve as essential tools for finger fracture recovery, keeping broken bones properly aligned while healing occurs. By immobilizing the injured area, splints reduce pain and create optimal conditions for natural healing. The type of splint varies based on the fracture's location and severity - from simple tape supports to custom-made devices. Proper application is critical to ensure bones heal correctly without complications.
Medical professionals consider multiple factors when selecting splints: fracture type, location, and desired mobility during healing. They carefully position and secure splints to provide support without restricting blood flow. The right splint creates a stable environment that lets the body focus energy on repair processes.
Bracing for Support and Protection
Braces offer more flexibility than splints while still protecting injured fingers. They're commonly used for chronic conditions like arthritis or repetitive strain injuries. Modern braces can compress swollen areas, stabilize weak joints, or prevent further damage - all while allowing some movement. Many braces are customized for individual needs and specific injuries.
What makes braces valuable is their ability to protect while permitting controlled motion. This balance helps maintain joint flexibility during recovery. Adjustable features ensure proper fit and support throughout the healing process. When used correctly, braces significantly aid recovery by preventing re-injury while allowing gradual return to normal activities.
Exploring Physical Therapy Interventions: Tailored Exercises and Techniques
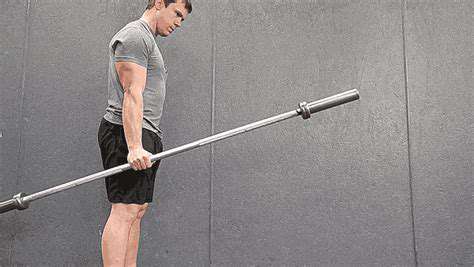
Tailored Exercise Programs for Specific Conditions
Physical therapists develop customized exercise plans based on each patient's diagnosis, abilities, and health status. These programs evolve as patients improve, starting gently and gradually increasing intensity. Therapists use various techniques - strength training, flexibility exercises, balance drills - all aimed at restoring normal function. Continuous monitoring ensures exercises remain effective and safe.
Programs might combine targeted strengthening with range-of-motion exercises and manual therapies. The ultimate goal extends beyond symptom relief - therapists equip patients with knowledge and skills for long-term management. Patients learn proper exercise techniques and understand why consistency matters for optimal results.
Manual Therapy Techniques and Modalities
Hands-on treatments address pain, stiffness, and mobility issues through specialized techniques. Therapists might use massage, joint mobilization, or careful manipulation based on individual needs. These methods improve joint function, reduce muscle tension, and enhance tissue flexibility. Effective treatment requires clear communication about comfort levels and treatment goals.
Therapists often complement manual techniques with therapeutic modalities. Options include heat/ice therapy, therapeutic ultrasound, or electrical stimulation - each serving specific purposes in the healing process. Heat relaxes tense muscles while cold reduces swelling. The therapist selects modalities based on the patient's condition and response to treatment, ensuring safe and effective care.
When Surgery Becomes Necessary: Understanding Surgical Options for Severe Cases
When Non-Surgical Treatments Fail
While many conditions respond well to conservative treatments, some require surgical intervention when other options don't work. This decision comes after careful evaluation of the condition's severity, patient health, and potential risks of continuing non-surgical approaches. Medical teams thoroughly assess all factors before recommending surgery.
Exploring the Spectrum of Surgical Procedures
Modern surgery offers options ranging from minimally invasive techniques to traditional open procedures. The choice depends on the specific condition, its complexity, and desired outcomes. Minimally invasive methods typically mean less pain and faster recovery, while complex cases may need more extensive approaches. Surgeons explain all options so patients can make informed decisions.
Evaluating the Risks and Benefits
All surgeries carry some risk, from minor complications like temporary swelling to more serious concerns. Doctors thoroughly discuss potential risks versus expected benefits for each procedure. This conversation considers the patient's overall health and how the surgery might improve their quality of life.
Understanding the Recovery Process
Post-surgery rehabilitation plays a crucial role in successful outcomes. Recovery timelines vary based on procedure complexity and individual healing rates. Patients receive detailed instructions about activity restrictions, wound care, and rehabilitation exercises. Following these guidelines carefully helps ensure optimal healing.
Surgical Alternatives and Complementary Therapies
Some patients benefit from combining surgery with other therapies. Nutritional support, stress reduction techniques, or specialized medical treatments might enhance surgical results. Healthcare teams help patients explore options that complement their surgical plan for comprehensive care.
The Importance of Open Communication and Informed Consent
Clear doctor-patient communication forms the foundation of successful surgical care. Patients should understand their condition, all treatment options, and what to expect from surgery. Asking questions and discussing concerns helps patients feel confident in their decisions. This collaborative approach leads to better outcomes and patient satisfaction.