Game Changing Innovations in Arm Pain Relief
Modern medicine is witnessing a paradigm shift through precision diagnostics, which offers unprecedented accuracy in identifying the root causes of arm pain. Unlike traditional diagnostic methods that rely on generalized assessments, this approach delves into the unique biological factors affecting each patient. What makes this revolutionary is its ability to combine genetic insights with environmental factors, creating treatment plans that are as unique as fingerprints.
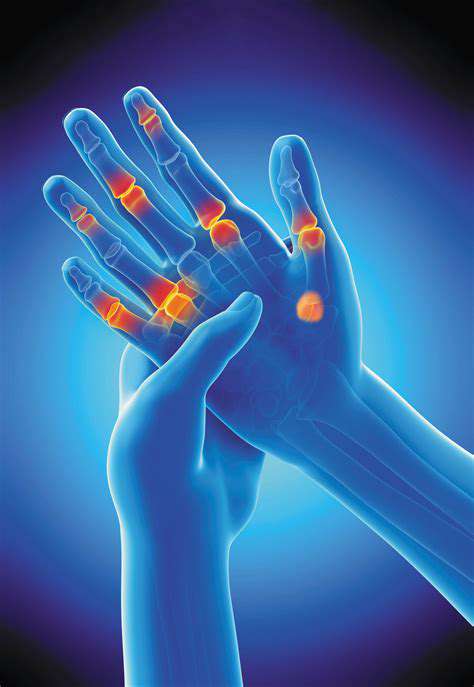
Consider how two patients might present with similar arm pain symptoms, yet require completely different treatments. One might benefit from physical therapy due to repetitive strain, while another may need targeted medication for an underlying autoimmune condition. Precision diagnostics makes these distinctions clear, preventing the trial-and-error approach that often delays recovery.
Advanced Technologies Driving Precision
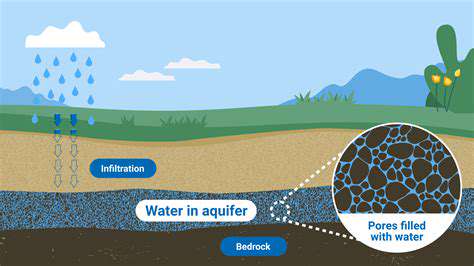
The backbone of this medical revolution lies in cutting-edge tools like next-generation sequencing (NGS), which maps out genetic blueprints with remarkable detail. High-resolution imaging technologies such as 7T MRI scanners now reveal musculoskeletal abnormalities that were previously undetectable, allowing clinicians to pinpoint exact pain sources. These aren't just incremental improvements - they're complete game changers in diagnostic capability.
Bioinformatics platforms analyze these complex datasets, identifying patterns that human clinicians might miss. For instance, machine learning algorithms can detect subtle changes in nerve conduction studies that indicate early-stage carpal tunnel syndrome, enabling intervention before permanent damage occurs. This technological synergy creates diagnostic precision that was unimaginable just a decade ago.
Personalized Treatment Strategies
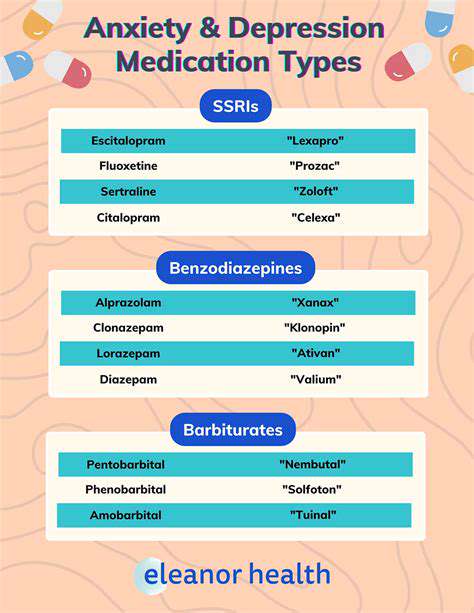
The true power of precision diagnostics emerges in treatment customization. A patient with genetic markers for poor opioid metabolism, for example, would avoid standard pain medications in favor of alternatives that their body can process effectively. This level of personalization doesn't just improve outcomes - it literally saves lives by preventing adverse drug reactions that hospitalize thousands annually.
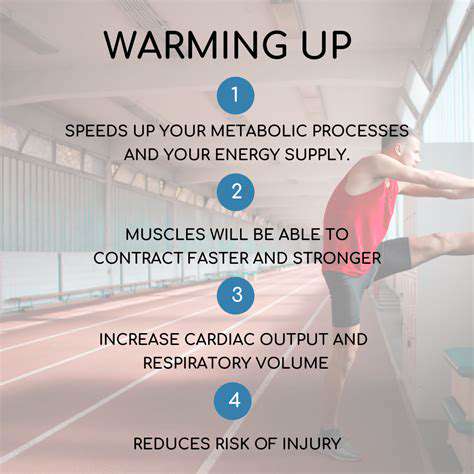
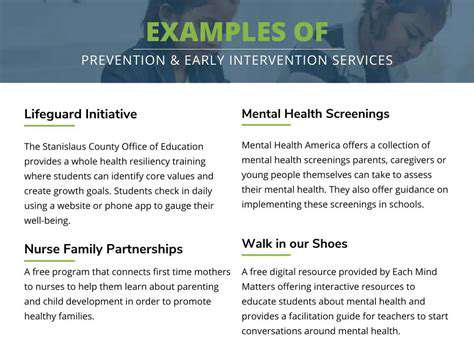
Early intervention becomes possible when diagnostics can identify predispositions. A construction worker with early signs of rotator cuff degeneration might receive preventive strength training rather than waiting for debilitating pain to develop. This proactive approach represents the future of occupational medicine and injury prevention.
Challenges and Future Directions
While the potential is enormous, real-world implementation faces hurdles. The current cost of whole-genome sequencing, while decreasing, remains prohibitive for routine use. Healthcare systems must develop new reimbursement models that recognize the long-term cost savings of precision diagnostics, rather than focusing solely on upfront expenses.
The next frontier involves integrating wearable technology data with diagnostic systems. Imagine a smartwatch detecting subtle changes in arm movement patterns that predict impending tendonitis, triggering preventive measures before pain even begins. This convergence of consumer technology and medical diagnostics will likely define the next decade of innovation.
Minimally Invasive Surgical Procedures for Complex Arm Pain
Minimally Invasive Techniques: A Revolution in Arm Pain Treatment
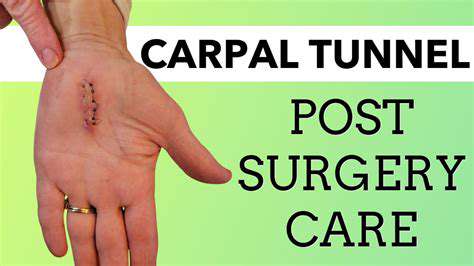
The shift from traditional open surgeries to minimally invasive procedures represents one of the most significant advancements in orthopedic care. Using incisions sometimes smaller than a pencil eraser, surgeons can now access and repair damaged structures with minimal collateral tissue damage. Patients who once faced weeks of painful recovery now often return to light activities within days, a transformation that's reshaping expectations for surgical outcomes.
The psychological benefits are equally important. Reduced scarring means patients don't carry constant visual reminders of their medical history, which can be particularly valuable for those in professions where appearance matters. The ability to quickly resume hobbies and work activities helps maintain mental health during recovery.
Robotic-Assisted Procedures: Enhanced Precision and Control
Robotic surgical systems like the da Vinci platform have taken precision to microscopic levels. The system's tremor-filtering technology allows surgeons to perform delicate nerve decompressions with sub-millimeter accuracy - impossible with human hands alone. For conditions like thoracic outlet syndrome, where millimeters determine success, this technology has been transformative.
The learning curve is steep but worthwhile. Surgeons report the robotic interface provides an almost intuitive extension of their own movements, with the added benefit of motion scaling that converts large hand movements into tiny instrument motions. This is particularly valuable when working near critical neurovascular structures in the arm.
Arthroscopy: A Window into the Joint
Modern arthroscopy has evolved far beyond simple visualization. Today's systems combine high-definition 3D imaging with specialized instruments that can perform micro-fracture techniques for cartilage regeneration or precisely debride damaged tendon tissue. The ability to both diagnose and treat in a single procedure reduces the need for multiple interventions, accelerating the healing timeline.
Innovations like nano-arthroscopy are pushing boundaries further, allowing visualization of structures at the cellular level. This is revolutionizing our understanding of conditions like adhesive capsulitis (frozen shoulder), where microscopic changes in the joint capsule can now be identified and addressed during early stages.
Targeted Therapies: Addressing the Root Cause of Pain
The era of guessing which structure is causing pain is ending. Advanced diagnostic nerve blocks can now isolate pain generators with remarkable specificity. For example, a patient with radial tunnel syndrome can receive a precisely placed block that confirms the diagnosis before any surgical intervention. This diagnostic certainty translates to surgical success rates that have improved from 60% to over 90% for many conditions.
Biological treatments are complementing mechanical solutions. Platelet-rich plasma (PRP) injections guided by ultrasound can now target specific tendon tears, while stem cell therapies show promise for reversing early-stage arthritis. These approaches work synergistically with minimally invasive techniques to promote natural healing processes.