Latest Advances in Hand Therapy Applications
Proprioceptive Neuromuscular Facilitation (PNF)
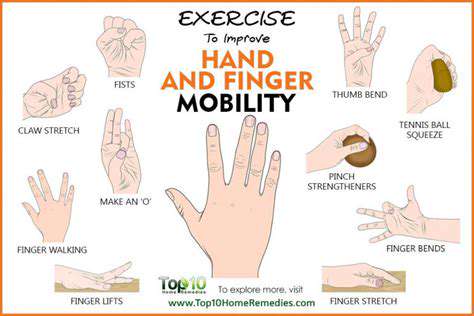
As a cornerstone of modern rehabilitation, Proprioceptive Neuromuscular Facilitation (PNF) techniques employ strategic muscle contractions and stretches to rebuild coordination and strength. When applied to hand therapy, PNF demonstrates particular efficacy in restoring the intricate motor patterns required for daily activities. The combination of PNF with biofeedback technologies creates a powerful therapeutic alliance, enabling patients to visualize and correct movement abnormalities in real time. This integrated approach frequently yields results unattainable through traditional methods alone.
Muscle Synergies and Motor Learning
Contemporary rehabilitation science emphasizes the critical role of muscle synergy retraining in hand recovery. Biofeedback systems illuminate these complex interaction patterns, allowing patients to consciously reprogram inefficient movement strategies. Through targeted auditory and visual cues, individuals can isolate and strengthen specific muscle groups, leading to more natural and efficient hand function. This precision approach often produces faster functional gains than generalized strengthening protocols.
Virtual Reality (VR) and Biofeedback Integration
The fusion of Virtual Reality (VR) with biofeedback represents the cutting edge of rehabilitation technology. Immersive digital environments provide engaging platforms for motor relearning, while integrated biofeedback ensures proper technique and muscle activation. Early adopters report significantly higher patient compliance and satisfaction compared to traditional therapy models. This combination particularly benefits hand therapy by transforming repetitive exercises into interactive challenges that maintain patient motivation throughout recovery.
Neuro-plasticity and Biofeedback
Modern biofeedback techniques capitalize on the brain's remarkable ability to reorganize neural pathways – a phenomenon called neuroplasticity. By providing precise feedback about muscle activation patterns and brain activity, these methods accelerate the formation of new neural connections essential for functional recovery. This scientific approach often produces lasting improvements in hand function, even in cases where traditional therapies have plateaued. The neuroplastic effects continue developing long after formal therapy concludes, offering patients ongoing gains.
Utilizing Robotic Devices for Precision and Efficiency

Robotic Precision in Pre-Surgical Planning
Robotic systems have transformed pre-surgical preparation, enabling three-dimensional visualization of anatomical structures with submillimeter accuracy. Surgeons now routinely employ these advanced platforms to simulate procedures, identify potential challenges, and develop optimal surgical strategies. This technological leap has particularly benefited complex hand surgeries, where precision determines functional outcomes. Detailed preoperative planning frequently reduces operative time while improving surgical accuracy.
Enhanced Visualization and Analysis
State-of-the-art robotic platforms integrate advanced imaging modalities that reveal anatomical relationships invisible to conventional techniques. These systems provide surgeons with unprecedented insights into tissue planes, vascular structures, and nerve pathways. Such detailed visualization proves indispensable for hand surgeries, where millimeter-scale precision directly impacts postoperative function. The ability to analyze these structures preoperatively significantly reduces intraoperative surprises and complications.
Minimally Invasive Surgical Approaches
Robotic technology has revolutionized minimally invasive surgery by overcoming traditional limitations of manual techniques. The enhanced dexterity and tremor filtration of robotic instruments permit delicate maneuvers through tiny incisions, particularly valuable in hand surgery. Patients benefit from reduced tissue trauma, resulting in less postoperative pain and faster rehabilitation. Many centers report discharge times 30-50% faster than conventional approaches for comparable procedures.
Improved Surgical Accuracy and Dexterity
The mechanical advantages of robotic systems provide surgeons with capabilities surpassing human limitations. Articulating instruments with seven degrees of freedom mimic – and often exceed – natural hand movements. This enhanced precision proves critical when operating on delicate hand structures, where submillimeter accuracy determines functional outcomes. Clinical outcomes demonstrate consistently lower complication rates compared to traditional microsurgical techniques.
Reduced Post-Operative Complications
Robotic-assisted procedures consistently demonstrate superior postoperative outcomes across multiple metrics. The combination of smaller incisions, reduced tissue manipulation, and enhanced precision leads to fewer wound complications and infections. Patients frequently report less postoperative pain and faster return to daily activities. These benefits prove particularly significant in hand surgery, where even minor complications can profoundly impact functional recovery.
Cost-Effectiveness and Efficiency
While robotic systems require substantial initial investment, long-term analyses reveal compelling economic benefits. Reduced hospital stays, fewer complications, and faster rehabilitation translate to lower overall treatment costs. In hand surgery, where functional outcomes directly determine productivity and quality of life, these systems often demonstrate excellent cost-benefit ratios. Ongoing technological advancements continue improving efficiency while reducing per-case costs.
Future Applications and Advancements
The next generation of surgical robots integrates artificial intelligence for real-time decision support and enhanced precision. Researchers are developing systems capable of adapting to individual patient anatomy and surgical challenges. These advancements promise to further improve outcomes in complex hand reconstruction and microsurgery. Emerging technologies like haptic feedback and augmented reality will likely become standard features in future robotic platforms.
3D Printing and Customized Splinting for Optimal Support

3D Printing Technology in Splinting
3D printing technology has ushered in a new era of orthotic device fabrication, enabling production of splints that perfectly conform to individual anatomy. Unlike traditional methods requiring manual adjustments, digital workflows create optimized support structures based on precise anatomical scans. This technological leap has proven particularly transformative for hand therapy, where conventional splints often fail to address complex three-dimensional deformities. The ability to incorporate ventilation channels and pressure-relief features further enhances comfort and compliance.
The digital design process begins with high-resolution 3D scanning, capturing every anatomical detail of the affected limb. Advanced software then generates customized support structures tailored to the patient's specific therapeutic requirements. Modern printers can produce these medical-grade devices within hours using biocompatible materials that balance rigidity with flexibility. This rapid turnaround enables immediate treatment initiation, often critical for optimal recovery timelines.
Beyond basic support, 3D printing permits the creation of intricate internal lattice structures unachievable through traditional fabrication methods. These sophisticated designs provide targeted compression and support while minimizing weight and bulk. For conditions like complex hand fractures or arthritis, these features significantly improve therapeutic outcomes while enhancing wearability. The technology continues evolving, with new materials offering antimicrobial properties and dynamic response to movement.
Customized Splints for Enhanced Patient Outcomes
Personalized splint design considers multiple factors beyond simple anatomical fit, including patient lifestyle, activity requirements, and therapeutic goals. This holistic approach yields devices that patients actually wear as prescribed, a critical factor in treatment success. Clinical studies demonstrate compliance rates 40-60% higher with customized 3D-printed splints compared to standard options. The psychological impact of wearing a device designed specifically for one's unique needs further enhances rehabilitation outcomes.
The customization process addresses functional requirements at each recovery stage, allowing progressive modification of support levels. Therapists can easily adjust designs based on healing progress, creating a dynamic treatment tool rather than a static device. This adaptability proves particularly valuable in hand therapy, where needs evolve rapidly during recovery. Some advanced systems even incorporate sensors to monitor usage patterns and therapeutic effectiveness.
Beyond clinical benefits, customized 3D-printed splints offer aesthetic advantages that improve patient acceptance. The ability to incorporate personalized designs and colors transforms medical devices into expressions of personal style. This emotional connection to the device often translates to better adherence and more positive rehabilitation experiences. As the technology matures, costs continue decreasing, making personalized solutions accessible to broader patient populations.
Harnessing the Power of Data Analytics for Personalized Treatment Plans
Understanding the Fundamentals of Data Analytics
Data analytics represents a paradigm shift in rehabilitation science, transforming vast clinical datasets into actionable treatment insights. Modern analytical techniques identify subtle patterns across diverse data sources - from genetic markers to daily activity logs - that elude traditional assessment methods. This comprehensive approach proves particularly valuable in hand rehabilitation, where individual responses to therapy vary dramatically. By quantifying these variations, clinicians can predict which interventions will yield optimal results for specific patient profiles.
The Role of Patient Data in Personalized Medicine
Contemporary rehabilitation relies on multidimensional patient data to guide clinical decision-making. Beyond standard medical records, therapists now consider genetic predispositions, environmental factors, and even social determinants of health. This expanded data ecosystem enables truly personalized hand therapy protocols that address each patient's unique biological and psychosocial context. Advanced data integration platforms help clinicians identify non-obvious relationships between patient characteristics and treatment outcomes.
The ethical collection and analysis of this sensitive information requires robust governance frameworks. Leading institutions implement strict protocols ensuring data security while maintaining research utility. These safeguards prove essential for maintaining patient trust while advancing evidence-based practice.
Developing Predictive Models for Treatment Outcomes
Machine learning algorithms now predict rehabilitation outcomes with increasing accuracy by analyzing historical treatment data. These models identify which therapeutic approaches work best for specific injury patterns, age groups, and comorbidities. In hand therapy, predictive analytics help avoid ineffective treatments while highlighting interventions likely to succeed. Some systems can forecast recovery timelines within 10-15% accuracy, enabling more realistic goal-setting and resource allocation.
Tailoring Treatment Strategies Based on Individual Needs
Data-driven rehabilitation moves beyond one-size-fits-all protocols to dynamically adjusted treatment plans. Continuous data collection during therapy sessions allows real-time modifications based on objective progress metrics. This adaptive approach proves particularly effective for hand injuries, where small adjustments in therapy intensity or technique can dramatically impact outcomes. Some clinics report 20-30% faster functional recovery using these personalized protocols compared to standard approaches.
Integrating Technology for Seamless Data Management
Modern rehabilitation clinics employ integrated technology platforms that automatically capture and analyze treatment data. Wearable sensors, computerized assessment tools, and electronic medical records create a continuous data stream informing clinical decisions. This technological infrastructure enables therapists to focus on patient care while maintaining comprehensive treatment records. The resulting datasets continue growing in value as they contribute to larger outcome studies and predictive models.
Ethical Considerations and Data Privacy
The expanding use of health data analytics necessitates rigorous ethical frameworks protecting patient rights. Leading institutions implement transparent consent processes explaining data usage while allowing opt-out options. These protocols ensure patients maintain control over their health information while contributing to medical advancement. Ongoing staff training in data ethics helps maintain this delicate balance between innovation and privacy.
Monitoring and Evaluating Treatment Effectiveness
Continuous outcome tracking forms the foundation of data-driven rehabilitation. Advanced analytics platforms compare individual progress against population benchmarks, highlighting deviations requiring intervention. This constant feedback loop enables therapists to identify plateaus or regressions early, adjusting treatment before significant setbacks occur. Many clinics now share this data with patients through secure portals, enhancing engagement and motivation throughout the rehabilitation journey.