Next Generation Treatments for Wrist Arthritis
Recent clinical observations highlight how this technology changes treatment paradigms. Patients who previously discontinued medications due to intolerable effects now maintain therapy successfully, thanks to dramatically reduced systemic exposure. This advancement opens new possibilities for using potent medications that were previously considered too risky for long-term arthritis management.
Enhanced Drug Stability and Bioavailability
Contemporary DDS platforms incorporate sophisticated mechanisms to protect medications from premature breakdown while ensuring optimal delivery timing. These systems maintain drug integrity during transit through the body, releasing active compounds precisely when and where they're needed most. The result? More consistent therapeutic effects with fewer peaks and valleys in medication availability.
This technological leap proves especially valuable for arthritis medications with narrow therapeutic windows. By smoothing out drug release patterns, DDS platforms minimize toxicity risks while maximizing beneficial effects. Patients benefit from steadier symptom control without the rollercoaster of fluctuating drug levels that often plagues traditional administration methods.
Novel Biomaterials for Joint Replacement and Augmentation
Biocompatibility and Material Selection
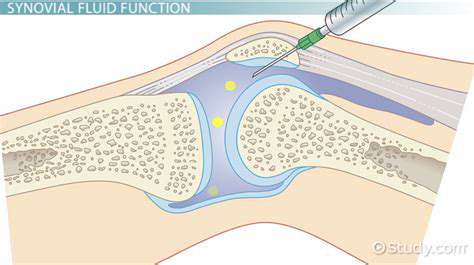
The quest for better joint solutions has led to remarkable innovations in biocompatible materials. Today's researchers evaluate potential substances through rigorous testing, examining how they interact with living tissues at microscopic levels. Advanced surface treatments now enable materials to communicate with surrounding cells, encouraging natural integration rather than triggering defensive reactions.
Current developments focus on creating smart interfaces where implant surfaces actively promote tissue bonding. These next-generation materials incorporate biological signals that guide cell behavior, potentially reducing recovery times and improving long-term implant stability. Such innovations represent a significant departure from earlier approaches that simply sought to minimize negative reactions.
Mechanical Properties and Design
Joint replacement materials must withstand extraordinary demands while mimicking natural movement patterns. Engineers now employ advanced simulation tools to predict how novel materials will perform under years of use, accounting for factors like repetitive stress and environmental changes within the body. The ideal material combines strength with just enough flexibility to prevent stress shielding - a phenomenon where implants absorb too much load, causing surrounding bone to weaken.
Modern design philosophy emphasizes anatomical accuracy, with implants tailored to individual patient characteristics. Digital modeling allows for precise customization, ensuring optimal fit and function. This personalization extends to material selection, with different implant regions potentially incorporating varied substances to best match local biomechanical requirements.
Manufacturing Techniques and Processing
The manufacturing revolution in joint implants centers on additive techniques that build components layer by layer. This approach enables intricate internal structures that promote bone ingrowth while maintaining exterior precision. Quality control has similarly advanced, with real-time monitoring systems ensuring each implant meets exacting standards throughout production.
Post-processing treatments now enhance material performance in ways previously unimaginable. Surface texturing at nano-scales, combined with bioactive coatings, creates implants that actively participate in the healing process rather than simply serving as passive replacements. These advancements blur the line between artificial and natural joint components.
Clinical Trials and Evaluation
Contemporary implant evaluation extends far beyond initial safety assessments. Longitudinal studies now track patients for decades, gathering detailed data on wear patterns, biological responses, and functional outcomes. This wealth of information feeds back into design improvements, creating a continuous cycle of refinement.
New evaluation methods provide unprecedented insights into implant performance. Advanced imaging techniques reveal microscopic interactions at the bone-implant interface, while sensor-equipped prototypes collect real-world usage data. These tools help researchers understand not just whether implants work, but how and why they succeed or fail in various scenarios.
Future Directions and Challenges
The horizon of joint replacement technology includes bioresorbable scaffolds that gradually transfer load to regenerating natural tissue. Researchers are exploring materials that can change properties in response to physiological conditions, providing dynamic support throughout the healing process. The integration of diagnostic capabilities into implants represents another exciting frontier, enabling continuous monitoring of joint health.
Scaling these advanced technologies while maintaining affordability presents significant challenges. The field must balance innovation with accessibility, ensuring that breakthroughs benefit all patients rather than becoming exclusive options. Material scientists collaborate with health economists to develop solutions that deliver maximum value throughout the healthcare system.
The Future of Wrist Arthritis Treatment: Combining Approaches for Optimal Outcomes
Minimally Invasive Procedures
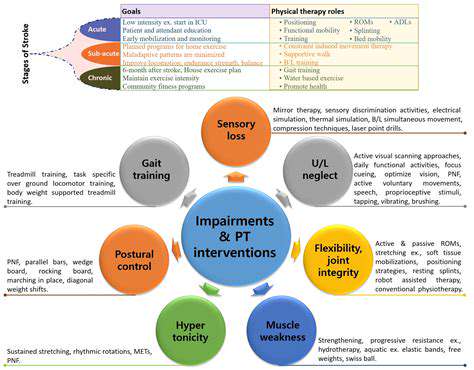
Contemporary wrist surgery emphasizes preservation over sacrifice. Surgeons now employ techniques that repair rather than replace, using specialized instruments that minimize collateral damage. This philosophy extends to postoperative care, with rehabilitation protocols designed to capitalize on the body's natural healing capacity.
Advanced visualization systems provide surgeons with magnified, high-definition views of wrist anatomy, enabling interventions with sub-millimeter precision. Combined with computer navigation, these tools allow for corrections tailored to each patient's unique biomechanics. The result? Procedures that address pathology while preserving maximum natural function.
Pharmacological Innovations
The next generation of arthritis medications moves beyond symptom suppression to target underlying disease mechanisms. Researchers are developing compounds that interrupt specific inflammatory pathways while sparing protective biological processes. These precision pharmaceuticals aim to break the cycle of joint degeneration rather than simply masking its effects.
Novel delivery methods enhance these pharmacological advances. Sustained-release formulations provide consistent medication levels, while targeted delivery systems concentrate drugs in affected joints. This combination of smart molecules and intelligent delivery promises to transform medical management of wrist arthritis.
Biologics and Regenerative Therapies
Regenerative approaches harness the body's innate repair capabilities, using concentrated growth factors and stem cells to stimulate tissue renewal. While still evolving, these techniques show particular promise for early-stage arthritis where significant cartilage remains. Clinical protocols now emphasize precise preparation and application methods to maximize therapeutic potential.
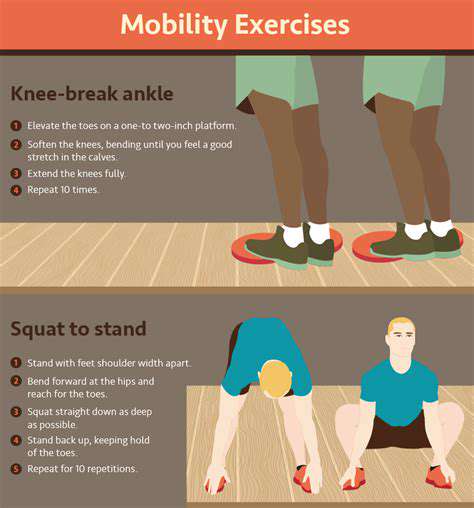
Combination therapies that pair biologics with mechanical stimulation demonstrate synergistic effects. Specialized rehabilitation devices apply controlled forces to treated joints, creating an environment conducive to tissue regeneration. This marriage of biological and physical approaches represents a holistic strategy for joint restoration.
Non-Surgical Management Strategies
Modern conservative care integrates evidence-based modalities in personalized combinations. Therapists now employ motion analysis to design exercise programs that protect vulnerable joints while maintaining function. Activity modification strategies help patients maintain independence by adapting rather than eliminating valued pursuits.
Advancements in orthotic design provide support without restricting necessary movement. Smart materials in braces adjust stiffness based on activity level, offering protection during demanding tasks while allowing freedom during gentle motions. These dynamic solutions help patients stay active without exacerbating joint damage.
Technology-Driven Diagnostics and Monitoring
Diagnostic precision has reached new levels with quantitative imaging techniques that detect subtle biochemical changes before structural damage occurs. Advanced ultrasound modalities visualize soft tissue inflammation with remarkable clarity, while functional MRI sequences reveal how joints behave under load.
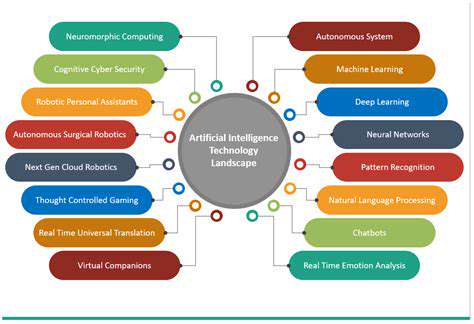
Wearable technology provides continuous monitoring outside clinical settings, capturing real-world joint performance data. Machine learning algorithms analyze these datasets, identifying patterns that predict flare-ups or progression. This proactive approach enables timely intervention before irreversible damage occurs.
Personalized Treatment Approaches
The era of one-size-fits-all arthritis management has given way to precision medicine. Treatment algorithms now incorporate genetic markers, biomarker profiles, and detailed joint imaging to guide decision-making. This individualized approach ensures patients receive the right combination of interventions at the optimal time in their disease course.
Multidisciplinary teams collaborate to create comprehensive care plans that address mechanical, biological, and psychosocial aspects of wrist arthritis. This holistic perspective recognizes that successful outcomes depend on more than just technical procedures - they require attention to the whole person and their unique life circumstances.