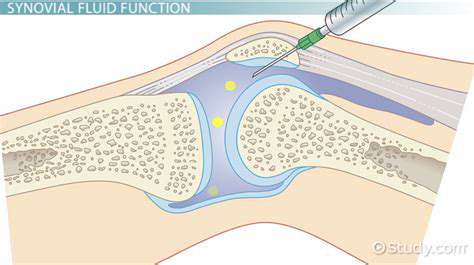
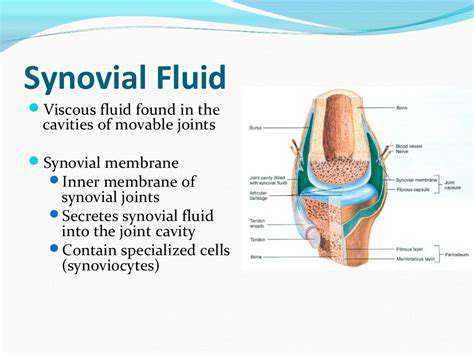
The Role of Synovial Fluid in Joint Health
This dual lubrication system adapts to different activity levels, explaining why both prolonged sitting and vigorous exercise can stress joints differently. The fluid's rheopectic properties mean its viscosity increases with shear rate, providing optimal protection across various movement speeds. Such sophisticated lubrication is unmatched by any artificial system.
Synovial Fluid's Nutrient Transport Function
Avascular articular cartilage relies entirely on synovial fluid for nutrient delivery and waste removal. The fluid's circulation during joint movement functions like a biological pump, forcing nutrients into cartilage matrix and flushing out metabolic byproducts. This mechanism explains why immobilization leads to cartilage degeneration while moderate exercise promotes joint health.
Oxygen and glucose diffuse from synovial capillaries into the fluid, then permeate cartilage under mechanical loading. Simultaneously, lactic acid and carbon dioxide move in the opposite direction. This exchange process highlights the fluid's critical role in maintaining cartilage viability despite its lack of direct blood supply.
Synovial Fluid's Immune Surveillance
The fluid contains specialized immune components that protect joints while avoiding excessive inflammation. Resident macrophages patrol the synovium, while soluble factors like complement proteins remain inactive until needed. This balanced immune presence allows rapid response to pathogens while preventing autoimmune attacks on joint tissues, a delicate equilibrium essential for long-term joint integrity.
During injury, the fluid's composition shifts dramatically as neutrophils and inflammatory cytokines enter from the bloodstream. This controlled inflammatory response facilitates tissue repair but must resolve completely to prevent chronic joint damage. The fluid's ability to modulate these immune processes demonstrates its sophisticated regulatory capacity.
Synovial Fluid's Shock Absorption Properties
The fluid's viscoelastic characteristics enable exceptional energy dissipation during impact loading. Under sudden compression, the fluid's viscosity increases dramatically, transforming joint spaces into hydraulic shock absorbers. This property protects cartilage from peak stresses that could otherwise cause microdamage, particularly important in weight-bearing joints during activities like running or jumping.
Simultaneously, the fluid's elastic components store and return some energy, improving movement efficiency. This combination of damping and energy return illustrates how synovial fluid contributes to both joint protection and mechanical performance during dynamic activities.
Conditions Affecting Synovial Fluid and Joint Health
Factors Influencing Synovial Fluid Viscosity
Synovial fluid viscosity represents a critical parameter determining joint function. The fluid's rheological properties depend on multiple interacting factors including molecular weight of hyaluronic acid, protein content, and temperature. Even small changes in hyaluronan concentration can dramatically alter lubrication efficiency, explaining why viscosupplementation injections often help osteoarthritic joints.
Environmental factors like ambient temperature and atmospheric pressure subtly affect viscosity through molecular interactions. Similarly, hormonal fluctuations during menstrual cycles or pregnancy may temporarily modify fluid properties. These normal variations demonstrate the fluid's dynamic responsiveness to physiological conditions while maintaining essential functions.
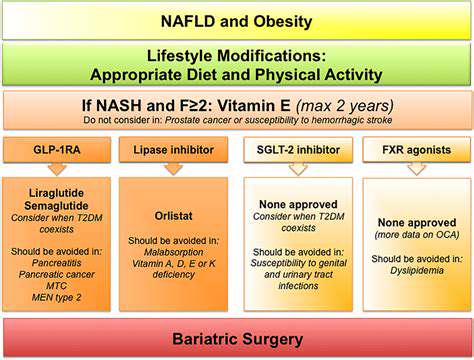
The Impact of Inflammation on Synovial Fluid
Inflammatory arthritis fundamentally alters synovial fluid composition and function. The influx of leukocytes increases fluid volume while degrading its lubricating molecules. Enzymes like matrix metalloproteinases break down hyaluronic acid and lubricin, creating a thinner, less effective lubricant that accelerates cartilage wear.
Simultaneously, inflammatory cytokines stimulate synovial cells to produce abnormal fluid components. This pathological fluid often contains immune complexes and autoantibodies that perpetuate joint damage. The resulting viscous cycle of inflammation and tissue destruction highlights why early intervention is crucial in inflammatory arthritis.
The Role of Nutrition in Synovial Fluid Health
Dietary components directly influence synovial fluid quality through multiple pathways. Essential fatty acids incorporate into synovial membranes, affecting fluid production and composition. Antioxidant nutrients help maintain hyaluronic acid integrity against oxidative stress, while vitamins C and D support collagen synthesis in adjacent tissues.
Hydration status significantly impacts synovial fluid volume and viscosity. Adequate water intake ensures proper fluid production, while dehydration concentrates synovial components, potentially impairing lubrication. These nutritional factors offer practical avenues for supporting joint health through lifestyle choices.
Age-Related Changes in Synovial Fluid
Progressive alterations in synovial fluid composition contribute to age-related joint degeneration. Synovial cells produce shorter hyaluronic acid chains with aging, reducing fluid viscosity and elasticity. This molecular aging parallels decreased cellular synthetic capacity throughout the body, reflecting broader biological aging processes.
Concurrently, cumulative mechanical wear alters joint biomechanics, changing fluid distribution patterns. These age-related changes create a predisposition to osteoarthritis but don't inevitably lead to symptoms, emphasizing the importance of preventive strategies throughout life.
Movement and Synovial Fluid Dynamics
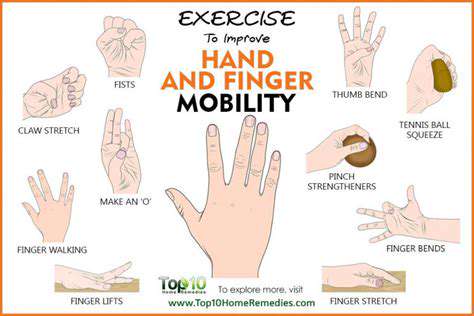
Joint motion drives essential synovial fluid circulation through multiple mechanisms. Compression-expansion cycles pump fluid through cartilage, while sliding motions distribute lubricants across surfaces. This mechanical stimulation also upregulates synovial cell activity, maintaining normal fluid production and composition.
Different movement patterns create varied fluid flow profiles, suggesting why diverse exercise may benefit joints more than repetitive motions. The fluid's responsiveness to mechanical input explains the therapeutic value of carefully prescribed movement for joint disorders, balancing loading and recovery.