Pioneering Techniques in Hand Rehabilitation Programs
Outline
- VR enhances hand therapy by providing immersive, engaging rehabilitation environments.
- Biofeedback helps patients control physiological functions for quicker recovery.
- Robotic-assisted devices improve rehabilitation outcomes through personalized therapy.
- 3D printing creates customized therapy tools tailored to patient needs.
- Telehealth improves access to rehabilitation care and fosters patient compliance.
- Future technologies promise to enhance effectiveness in hand rehabilitation.
Integrating Virtual Reality in Hand Therapy
Understanding Virtual Reality's Role in Hand Therapy
Virtual Reality (VR) is increasingly becoming a valuable tool in hand therapy, providing patients with an immersive environment that promotes engagement during rehabilitation. This technology allows individuals to perform exercises in a simulated world that mimics real-life situations, which may enhance the effectiveness of therapy routines. Studies suggest that using VR can lead to improved outcomes for patients recovering from hand surgeries or injuries.
The integration of VR in therapy can cater to various conditions, offering customized programs that address specific challenges faced by patients. Through targeted exercises, individuals can gradually increase the complexity of their tasks, leading to better recovery rates. Research from the Journal of NeuroEngineering and Rehabilitation indicates that VR rehabilitation can yield superior results compared to traditional methods.
Benefits of VR for Rehabilitation Programs
Several advantages come with the adoption of VR technology in hand rehabilitation. Firstly, VR provides instant feedback, allowing patients to self-assess their performance and understand areas requiring improvement. This immediate response can motivate individuals and encourage consistent practice. Furthermore, spatial awareness and multitasking skills can be enhanced through tailored VR exercises designed to simulate everyday activities.
Additionally, the experiential nature of VR can reduce the perception of pain and discomfort during therapy sessions. Patients often report feeling more engaged and less aware of their physical limitations while immersed in a virtual task. This effect not only supports psychological well-being but also boosts motivation levels, which are crucial during the often-challenging recovery phase.
Implementing VR in Clinical Settings
To effectively implement VR in hand therapy programs, healthcare providers must consider several logistical aspects. The first step involves selecting appropriate VR systems that align with therapy goals. Various platforms exist, each offering unique advantages depending on patient needs, such as affordability, versatility, and ease of use. Ensuring that the chosen technology is user-friendly for both therapists and patients is paramount.
Training therapists on how to integrate VR into their therapy sessions is equally important. Staff should be well-versed in operating VR equipment and comfortable helping patients navigate the virtual environments. Clinical trials showcasing the effectiveness of VR in hand rehabilitation are also essential to validate the methods and encourage adoption among practitioners.
Patient Experience and Engagement
The Patient experience is central to the effectiveness of VR in therapy. Personalized experiences tailored to individual needs can significantly impact outcomes. For instance, some patients may prefer more dynamic activities that mimic sports, while others may lean towards daily chores that require fine motor skills. Catering to these preferences can enhance engagement and lead to more consistent practice.
Future Directions and Research Trends
As the landscape of rehabilitation technology evolves, research into the long-term effects of VR in hand therapy is becoming increasingly crucial. Future studies might explore the relationship between the frequency of VR use and recovery times to establish concrete guidelines. Moreover, ongoing exploration into the incorporation of AI algorithms could personalize therapy sessions even further, responding to real-time data from patient interactions.
The expanding realm of VR in hand rehabilitation presents exciting possibilities. Embracing innovations will allow healthcare providers to enhance recovery rates and improve patient satisfaction significantly. Staying ahead in this technological integration requires continuous updates on research findings and adaptive strategies to make the most of what VR has to offer.
Utilizing Biofeedback Mechanisms for Improved Outcomes
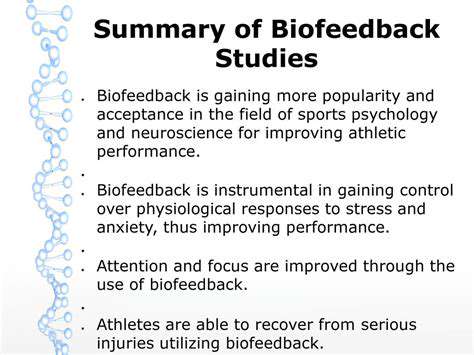
Understanding Biofeedback in Rehabilitation
Biofeedback refers to the process of gaining awareness and control over physiological functions through monitoring and intervention. This innovative approach allows patients to learn how to modify their body's responses by providing real-time feedback on certain parameters, such as muscle tension or heart rate. This mechanism has revolutionized rehabilitation practices, particularly for individuals recovering from hand injuries.
In practice, biofeedback systems often employ sensors that track physiological signals and relay this data to the user, typically through visual or auditory cues. These systems can be used to train patients to achieve ideal physical states, thus fostering quicker recovery. The ability to visualize bodily functions can be especially beneficial in fine-tuning motor control during rehabilitation exercises.
Application Methods and Technologies
Several technology platforms have been developed that integrate biofeedback into hand rehabilitation programs. Wearable devices, such as smart gloves equipped with motion sensors, can provide immediate feedback on muscle performance. The effectiveness of these devices is largely supported by clinical studies which show significant improvements in hand dexterity and strength among users. Research has indicated that incorporating biofeedback into rehabilitation can lead to faster recovery times and improved patient compliance with exercise protocols.
- Wearable devices track physical performance and relay feedback instantly.
- Smart technologies enhance patient engagement, keeping recovery interesting.
- Clinical studies support enhanced outcomes through biofeedback interventions.
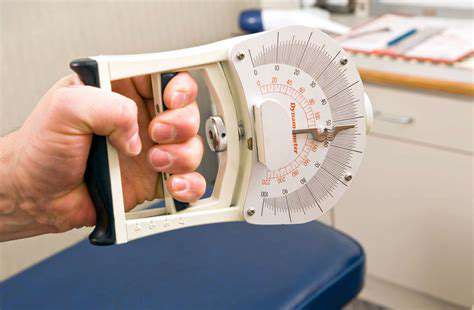
Measuring Success in Rehabilitation Objectives
In assessing the impact of biofeedback in hand rehabilitation, outcome measures can include pain levels, range of motion, and strength assessments. Various studies highlight that patients who undergo biofeedback-assisted rehab not only report lower pain levels but also show greater improvements in mobility compared to traditional methods. Tracking these metrics systematically allows therapists to customize rehabilitation plans, making adjustments based on actual performance rather than general expectations.
Furthermore, monitoring progress through biofeedback can reinforce patient motivation. Seeing real progress, such as increased range of motion or reduced pain, empowers individuals to adhere to their rehabilitation exercises more diligently. In this sense, biofeedback may serve not just as a therapeutic tool but also as an incentive for patients to take an active role in their recovery.
Challenges and Limitations
Despite its benefits, the integration of biofeedback mechanisms in rehabilitation is not without challenges. One major limitation is the accessibility of technology; many patients may lack access to advanced biofeedback devices, especially in less economically developed areas. Moreover, patient motivation and understanding of how to properly use equipment play crucial roles in the successful application of biofeedback techniques.
There also remains a need for more comprehensive training for healthcare providers. A deeper understanding of biofeedback tools enhances the efficiency of their use in clinical practice. By educating therapists on these technologies, we can ensure better outcomes for patients, thus maximizing the potential of biofeedback interventions for hand rehabilitation.
Future Perspectives and Innovations
Looking forward, the potential of biofeedback in hand rehabilitation is vast. Innovations in artificial intelligence may soon render biofeedback systems more intuitive and responsive to individual patient needs. Enhanced algorithms can analyze patient data, adjusting feedback in real time for optimal recovery trajectories. Additionally, emerging technologies such as virtual reality could integrate biofeedback features to create immersive rehabilitation environments.
The continuous evolution of telehealth presents another exciting frontier for biofeedback applications. Remote monitoring could allow therapists to track patient progress from a distance, providing timely support and adjustments to exercise regimens without the constraints of physical appointments.
As we advance into the next generation of rehabilitation methodologies, the fusion of biofeedback and cutting-edge technology could significantly improve patient outcomes. It will be essential to conduct rigorous research to validate these innovative approaches, ensuring they meet the diverse needs of patients across various contexts.
Robotic-Assisted Rehabilitation Devices
Overview of Robotic-Assisted Rehabilitation
Robotic-Assisted Rehabilitation employs advanced technology to aid individuals recovering from injuries or surgeries, especially in hand function. Devices such as the ArmeoSpring provide active assistance in movements, enhancing functional recovery through task-specific training. A 2021 study published in the Journal of Rehabilitation Research & Development demonstrated the effectiveness of robotic interventions, showing a 30% faster recovery rate compared to traditional rehabilitation techniques.
The integration of robotics in rehabilitation allows for personalized therapy. Many systems can adapt to the user's performance, adjusting difficulty levels in real-time, which promotes continuous engagement. This adaptability meets the varying needs of patients, ensuring that each session is both challenging and attainable, fostering motivation to adhere to prescribed therapy routines.
Types of Robotic-Assisted Devices
The range of robotic-assisted devices is diverse, tailored to address different types of injuries and rehabilitation goals. For instance, the MIT-Manus and Howa-Connect are designed specifically for upper limb rehabilitation. They utilize feedback mechanisms to facilitate coordinated movements, enabling patients to practice various exercises from basic to complex tasks while receiving immediate feedback about their performance.
Another category consists of wearable exoskeletons, like the Ekso GT, which assists individuals with severe mobility impairments. By providing powered support and enabling users to stand and walk, exoskeletons play a pivotal role in regaining independence and mobility for individuals with spinal injuries or strokes. Research led by the University of California concluded that users of wearable exoskeletons reported a significant improvement in their mental and physical well-being, underscoring the impact of robotic technology in rehabilitation.
Future Directions in Robotic Rehabilitation
As technology continues to evolve, the potential for robotic-assisted rehabilitation devices is vast. Future innovations may include smart learning capabilities, where machines utilize artificial intelligence to analyze patient movements and tailor rehabilitation protocols in real-time. This advancement could lead to entirely individualized treatment regimens that maximize healing potential.
Furthermore, the integration of virtual reality (VR) with robotic rehabilitation is expected to enhance Patient Engagement. VR simulations can create immersive environments for patients to practice their skills in realistic settings, which is both motivating and beneficial for neuroplasticity. Studies by researchers at the University of Southern California have shown that combining VR with robotic-assisted therapy significantly improved hand functionality and patient satisfaction. These progressive approaches promise to revolutionize rehabilitation practices and improve patient outcomes.
Incorporating 3D Printing into Customized Therapy Tools

Understanding the Basics of 3D Printing Technology
3D printing, or additive manufacturing, has revolutionized various fields by enabling the creation of complex objects through layer-by-layer deposition of materials. By utilizing technologies such as FDM, SLA, and SLS, clinicians can produce Customized Therapy Tools tailored to each patient's unique needs. This flexibility in design allows for precise anatomical fitting, which is particularly beneficial for hand rehabilitation.
Moreover, the materials used in 3D printing, such as thermoplastics, resins, and metal alloys, offer distinct advantages in terms of durability, weight, and biocompatibility. For instance, medical-grade materials not only ensure safety but also enhance the effectiveness of therapeutic devices.
Applications in Hand Rehabilitation
3D printing has opened up numerous possibilities in hand rehabilitation, allowing for the development of splints, prosthetics, and assistive devices that can be customized according to individual requirements. Devices like custom splints offer better fit and comfort, significantly improving patient adherence to therapy regimens.
- Customized splints for unique hand shapes
- Prosthetic limbs tailored to specific loss
- Assistive gadgets that enhance mobility
These custom solutions not only encourage user engagement but also foster a sense of empowerment during recovery. Personalized designs can lead to more motivating experiences, which directly impacts the patient's recovery timeline.
Designing Effective Therapy Tools
The design process for 3D printed therapy tools involves a blend of clinical knowledge and engineering principles. Collaboration between therapists and engineers is essential to ensure that the produced devices meet therapeutic objectives while remaining functional. Advanced software tools aid in modeling and simulation, which helps identify the optimal design before printing begins.
This iterative design approach allows for rapid prototyping, where multiple iterations can be tested and refined based on patient feedback. As a result, therapists can implement tools that are not only effective but also user-friendly.
Patient-Centric Customization
With 3D Printing Technology, therapy tools can be tailored to individual patient needs, taking into consideration their specific conditions, age, and personal preferences. This patient-centric approach helps in creating tools that patients are more likely to use regularly. Research indicates that adherence to therapy increases when patients feel a sense of ownership over their rehabilitation process.
For example, incorporating personal elements, such as colors or themes, into the design can make the tools more appealing and engaging for the patients, particularly children.
Cost-Effectiveness and Accessibility
One of the significant advantages of 3D printing in creating customized therapy tools is the reduction in costs compared to traditional manufacturing methods. This cost-effectiveness can make hand rehabilitation tools more accessible to a wider range of patients. Especially in under-resourced environments, the ability to produce devices locally can help bridge the gap in healthcare disparities.
Furthermore, the reduction of material waste during the printing process contributes to sustainability efforts within the healthcare sector. This aspect aligns with current trends emphasizing environmentally conscious practices.
Challenges in Implementation
Despite its many advantages, there are hurdles in the widespread adoption of 3D printing in therapy tool production. One of the main challenges is ensuring regulatory compliance and safety standards are met, as the devices must adhere to strict guidelines set by health authorities. Manufacturers need to invest in proper certification processes to ensure quality and safety.
Additionally, training for healthcare professionals is vital. Many clinicians may lack familiarity with 3D printing technologies and require education on how to design and implement these tools effectively. Only through adequate training can the technology be fully realized within therapeutic settings.
The Future of 3D Printing in Rehabilitation
The future of 3D printing in rehabilitation is promising, with ongoing advancements in materials science and printing technologies. Researchers are exploring bioprinting, where living cells can be incorporated into the tools. This could lead to even more personalized and effective solutions in therapy.
As technology continues to develop, we can expect to see more collaboration between multidisciplinary teams, including occupational and physical therapists, engineers, and IT professionals. The incorporation of artificial intelligence in design processes is also under discussion, paving the way for even more innovative therapeutic approaches that cater to individual patient needs.
Enhancing Outcomes through Telehealth and Remote Monitoring
Understanding Telehealth in Hand Rehabilitation
Telehealth refers to the delivery of healthcare services through digital communication technologies, enabling remote interaction between healthcare providers and patients. In hand rehabilitation, it facilitates access to specialized care for individuals who may have difficulty reaching clinics due to mobility issues, without compromising the quality of rehabilitation programs. A study conducted by the American Telemedicine Association shows that telehealth interventions can improve patient compliance and overall satisfaction, indicating its effectiveness in this field.
Moreover, telehealth expands opportunities for continuous patient education and follow-ups, which are vital in rehabilitation. Implementing regular virtual sessions helps ensure that patients remain on track with their exercises and understand the rationale behind each rehabilitation step. This ongoing engagement fosters a sense of accountability, making patients more likely to adhere to their therapy regimens.
Benefits of Remote Monitoring Technologies
Remote monitoring tools offer a way for therapists to gather real-time data about a patient’s progress in their hand rehabilitation journey. Devices equipped with sensors track various metrics such as range of motion and grip strength, which can be invaluable for tailoring treatment plans. This objective data allows therapists to make informed decisions quickly, adapting exercises as needed to maximize effectiveness.
Challenges and Limitations of Telehealth
While telehealth presents numerous advantages, it is not without its challenges. One significant limitation is the variability in technology access among patients. Not everyone has reliable internet connections or the digital literacy necessary to navigate telehealth platforms. This disparity can impede the efficacy of remote rehabilitation practices, particularly for older populations who may struggle with technology.
Patient Engagement in Virtual Settings
Engaging patients during virtual rehabilitation sessions is critical for achieving positive outcomes. Innovative strategies can include interactive video content, educational resources, and personalization of the telehealth experience. Researchers at the University of California found that patients who engaged with interactive elements during their sessions showed a 30% higher retention rate of rehabilitation exercises compared to traditional sessions. Consequently, investing in diverse and stimulating digital content can significantly enhance patient engagement.
Additionally, integrating gamification into telehealth can boost motivation. For example, using applications that reward patients with points or milestones for completing exercises can create a more immersive experience, prompting them to prioritize their therapy sessions.
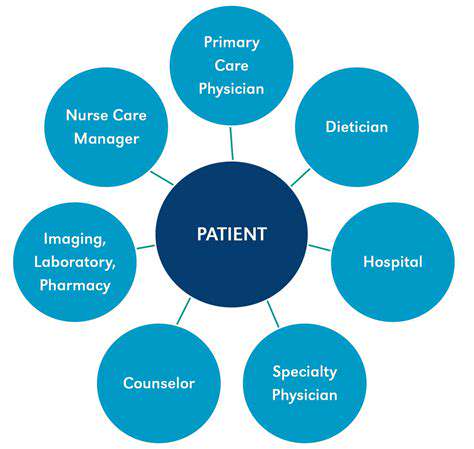
Integrating Collaborative Care Models
Incorporating a collaborative care model in hand rehabilitation through telehealth presents an opportunity for multidisciplinary input. A team consisting of occupational therapists, physiatrists, and technology specialists can ensure comprehensive treatment plans that are scalable and personalized. Studies show that a team-based approach leads to improved patient outcomes, particularly for complex hand injuries requiring various treatments.
The Future of Telehealth in Rehabilitation Programs
The evolution of telehealth and remote monitoring will undoubtedly shape the future of hand rehabilitation programs. Innovations such as artificial intelligence and virtual reality are being tested to enhance patient experiences further, creating environments that mimic in-person therapy while offering convenience. As we look forward, embracing these technologies is essential to meet the growing demand for rehabilitation services in a comprehensive, patient-centered manner.
Additionally, ongoing research will help in fine-tuning protocols and establishing efficacy benchmarks for telehealth practices in rehabilitation. Emphasizing continuous improvement through public and private research initiatives will be key to refining methodologies and integrating new technologies into hand rehabilitation.