Rehabilitation Protocols for Arm Fracture Recovery
Initial Immobilization
The initial phase of rehabilitation for an arm injury focuses primarily on immobilization to prevent further damage and allow the healing process to begin. This period of rest is crucial for reducing inflammation and pain. Immobilization typically involves the use of a sling, splint, or cast, depending on the specific injury and location. Proper immobilization techniques are essential to ensure the injured tissues heal in the optimal alignment for future function, and to prevent reinjury while the body is actively repairing the damage. This period also allows for the body to focus on the healing process and reduce any further strain on the injured area.
Careful monitoring of the affected area is critical during this immobilization period. Signs of infection, swelling that increases significantly, or persistent pain that isn't responding to prescribed pain management techniques should be immediately reported to a medical professional. Strict adherence to the prescribed immobilization period is vital for successful rehabilitation.
Pain Management Strategies
Managing pain effectively is essential throughout the rehabilitation process, particularly during the initial phase. Various pain management strategies can be employed, including over-the-counter pain relievers, prescribed medications, and physical therapies. These strategies help to reduce discomfort and promote a more comfortable healing environment. Understanding the different types of pain and their triggers is also important for developing effective pain management strategies.
Beyond medication, techniques like cold therapy and heat therapy can be incorporated into a pain management plan. Specific exercises and stretches, guided by a physical therapist, can also aid in pain management and promote healing. The goal is to find a combination of methods that effectively control pain while allowing for gradual, controlled movement and exercise.
Assessment of Injury Severity
An accurate assessment of the injury severity is paramount for developing an effective rehabilitation protocol. This evaluation considers the type of injury, the extent of tissue damage, and the affected area's range of motion. Factors like bone fractures, ligament tears, or muscle strains significantly impact the rehabilitation plan. The assessment helps in determining the appropriate level of immobilization, the necessary duration of the healing process, and the expected recovery time. This initial evaluation is also crucial for establishing realistic goals and expectations for the patient.
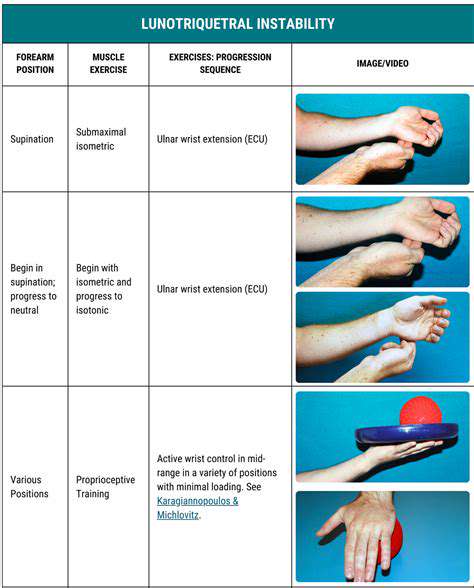
Early Range of Motion Exercises (AROM)
As the injury heals and pain subsides, carefully supervised early range-of-motion (AROM) exercises are introduced. These exercises, often guided by a physical therapist, help restore joint flexibility and prevent stiffness. Gentle movements are key during this phase, focusing on maintaining a pain-free range of motion. These exercises are crucial for promoting blood flow to the injured area and encouraging tissue regeneration. Careful attention to pain levels and proper technique is essential to avoid further injury.
Introducing Active Exercises (AROM and PROM)
Progressing from passive range-of-motion (PROM) exercises, active range-of-motion (AROM) exercises are introduced. These exercises involve the patient actively moving the affected arm, gradually increasing the range and intensity of the movement. As the healing progresses, the patient is encouraged to participate in active exercises, increasing the intensity and duration as tolerated. The rehabilitation process transitions from primarily passive to active involvement in the recovery. This gradual progression is essential for restoring strength, function, and overall mobility to the arm.
Strengthening and Functional Training
Once the range of motion and pain levels permit, strengthening exercises are incorporated into the rehabilitation program. These exercises focus on building the strength of the muscles surrounding the injured area, gradually progressing in intensity and complexity. This phase also involves functional training exercises that simulate real-life activities, such as lifting, carrying, and reaching. The goal is to restore the arm's full functional capacity, enabling the patient to perform everyday tasks without pain or limitations. Proper technique and gradual progression are key to preventing re-injury and optimizing recovery.
Long-Term Management and Prevention
Long-Term Physical Therapy
Following initial fracture healing, a crucial aspect of arm fracture recovery is long-term physical therapy. This phase focuses on restoring full range of motion, strength, and flexibility in the affected arm. Physical therapists will design personalized exercises to address specific needs and limitations, gradually increasing intensity and complexity as the patient progresses. This targeted approach helps prevent muscle atrophy, improve joint function, and enhance overall arm mobility, ensuring a complete recovery and minimizing long-term complications.
Regular sessions, often lasting 30-60 minutes, are essential for regaining strength and coordination lost during the immobilization period. Exercises will encompass a variety of movements, including active and passive range-of-motion exercises, resistance training using light weights or resistance bands, and balance and coordination drills. The goal is to gradually return the arm to its pre-injury functionality, ensuring the patient can perform daily tasks without pain or discomfort.
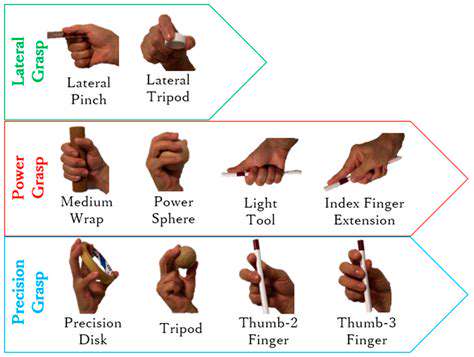
Ergonomic Modifications for Work and Home
To prevent re-injury and ensure optimal recovery, ergonomic adjustments in both the home and work environments are vital. This involves assessing current setups and implementing changes to reduce strain on the healing arm. For instance, at work, this might include adjusting desk height, chair position, and keyboard placement. At home, modifications could involve altering how tasks are performed, such as using assistive devices for cooking or using a different grip for household chores.
Proper ergonomics plays a critical role in long-term arm health. By minimizing repetitive stress and strain on the injured limb, individuals can significantly reduce the risk of re-injury and ensure sustainable recovery. Implementing these changes will facilitate a smoother transition back to daily activities and prevent potential complications associated with improper posture or repetitive movements.
Nutritional Support for Optimal Healing
Maintaining a balanced and nutritious diet is crucial for supporting the healing process and promoting overall well-being during arm fracture recovery. This includes consuming foods rich in protein, vitamins, and minerals, as these nutrients are essential for tissue repair and bone growth. Protein is particularly important for building and repairing muscle tissue, while vitamins and minerals contribute to overall immune function and bone health.
A diet rich in fruits, vegetables, lean proteins, and whole grains can provide the necessary nutrients. Furthermore, adequate hydration is essential for optimal bodily functions and plays a significant role in the healing process. Consulting with a registered dietitian can help tailor a personalized nutrition plan to meet individual needs and ensure the body receives the necessary nutrients for a complete recovery.
Preventing Recurrence and Long-Term Pain
While an arm fracture is a significant injury, preventative measures can help minimize the risk of recurrence and long-term pain. This includes maintaining proper posture and body mechanics, ensuring adequate rest periods to avoid overexertion, and using supportive devices, such as splints or braces, when engaging in strenuous activities. These precautions will help prevent re-injury and promote healthy tissue healing.
Regular check-ups with the orthopedic surgeon are essential to monitor the healing process and address any potential complications. Open communication with the medical team about any discomfort or concerns is crucial for preventing long-term pain and ensuring successful recovery. Following the prescribed rehabilitation protocol and lifestyle modifications are crucial in achieving optimal long-term outcomes.
Return to Activity and Sports
Returning to normal activities and resuming sports after an arm fracture requires a gradual and cautious approach. It's essential to listen to the body and avoid pushing the injured arm beyond its capabilities. A phased return to activity, monitored by the physical therapist, is crucial to prevent re-injury and ensure optimal recovery. This involves starting with light activities, gradually increasing intensity and duration as strength and range of motion improve.
The timeline for returning to sports and vigorous activities will vary depending on the severity of the fracture and the individual's recovery progress. Close collaboration with the orthopedic surgeon and physical therapist is vital to guide the patient through this process, ensuring a safe and successful transition back to their desired activities.
Managing Potential Complications
While most arm fractures heal without complications, some individuals may experience issues such as stiffness, weakness, or persistent pain. Addressing these potential complications promptly with the medical team is essential to ensure a smooth recovery. Early intervention and appropriate management can often prevent these issues from becoming chronic problems.
Stiffness in the joint can be managed through specialized exercises and stretches. Weakness in the muscles surrounding the fracture site can be addressed with targeted resistance training. Persistent pain can be managed through medication, physical therapy, and other pain management strategies. It is important to maintain open communication with the medical team to address any concerns or complications that arise during the recovery period.