Understanding Hand Joint Replacement: When Is It Necessary?
When is Hand Joint Replacement Necessary?
When Is Hand Joint Replacement Necessary?
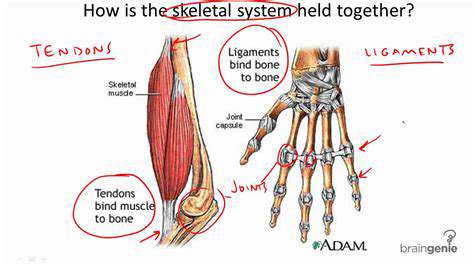
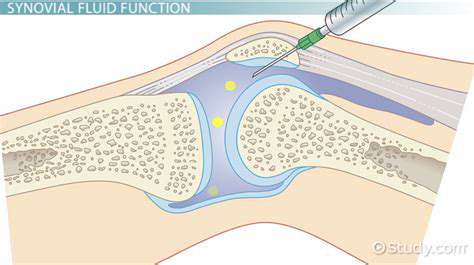
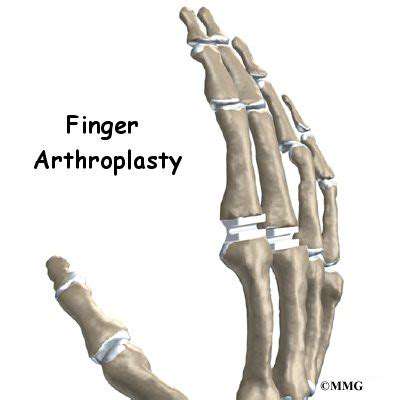
Hand joint replacement, also known as arthroplasty, is a surgical procedure that involves replacing a damaged or diseased joint in the hand with an artificial joint, or prosthesis. This procedure is typically considered when non-surgical treatments, such as medications, physical therapy, and splints, have failed to alleviate the pain and improve the function of the affected joint. It is crucial to understand that hand joint replacement isn't a first-line treatment and is reserved for severe cases where other options have proven ineffective.
Causes of Hand Joint Damage Requiring Replacement
Several conditions can lead to the deterioration of hand joints to the point where replacement is necessary. These include rheumatoid arthritis, osteoarthritis, and other forms of inflammatory arthritis. Trauma, such as fractures or dislocations, can also cause significant joint damage that may necessitate replacement. Additionally, certain genetic conditions or occupational overuse can contribute to the need for hand joint replacement.
Symptoms Indicating Potential Need for Replacement
Identifying the symptoms of hand joint damage is crucial for early intervention and potentially avoiding the need for replacement surgery. Persistent pain, especially with movement, is a common symptom. Stiffness in the affected joint, making it difficult to perform everyday tasks, is another indicator. Swelling and redness around the joint are also possible signs of underlying damage that could require replacement.
Types of Hand Joint Replacements Available
Different types of hand joint replacements are available, each tailored to the specific needs of the patient. These procedures vary depending on the specific joint being replaced. For instance, replacements for the metacarpophalangeal (MCP) joints may differ from those for the proximal interphalangeal (PIP) or distal interphalangeal (DIP) joints. Understanding the various types of prostheses and their potential benefits and limitations is crucial for informed decision-making.
Preoperative Considerations and Evaluations
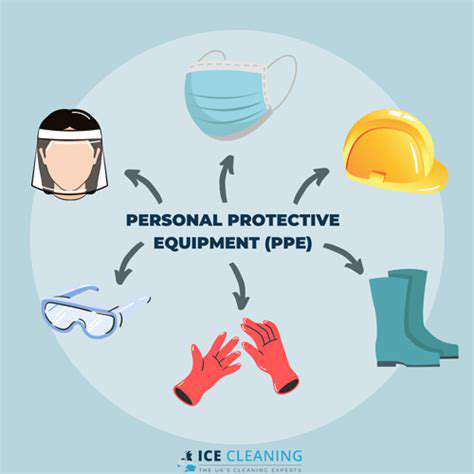
Prior to hand joint replacement surgery, a comprehensive evaluation is essential. This involves a thorough assessment of the patient's medical history, current health status, and the specific joint needing replacement. Diagnostic imaging, such as X-rays, CT scans, or MRIs, helps to determine the extent of the joint damage. The surgeon will discuss the procedure, potential risks, and expected outcomes with the patient to ensure they understand the process and are prepared.
Postoperative Recovery and Rehabilitation
Post-operative recovery involves a dedicated rehabilitation program. This typically includes physical therapy to regain range of motion, strength, and dexterity in the affected hand. The rehabilitation period can vary depending on the extent of the surgery and the patient's individual response. Patient compliance with the rehabilitation plan is crucial for successful outcomes and achieving optimal function.
Long-Term Outcomes and Considerations
Long-term outcomes of hand joint replacement can vary significantly. Factors such as the patient's overall health, the extent of the initial damage, and the skill of the surgical team all play a role. While hand joint replacement can significantly improve function and reduce pain, it's important to understand that the procedure is not a perfect solution for everyone. Potential complications and the need for ongoing follow-up care should be discussed with the surgeon.