Understanding the Causes of Hand Numbness and Weakness
Peripheral Nerve Entrapment
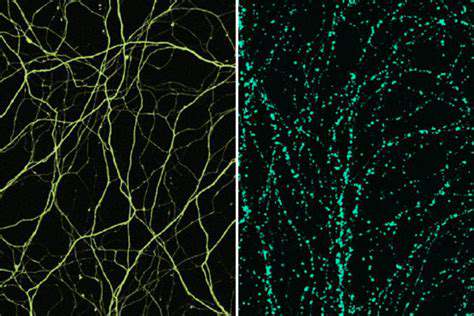
Peripheral nerve entrapment occurs when a nerve is compressed or squeezed by surrounding tissues, such as muscles, tendons, or bones. This compression can lead to a range of symptoms, including pain, numbness, tingling, and weakness in the affected area. The severity of the symptoms can vary depending on the degree of compression and the specific nerve involved. Understanding the location and nature of the entrapment is crucial for accurate diagnosis and effective treatment.
Common sites for entrapment include the carpal tunnel, where the median nerve is compressed, and the tarsal tunnel, where the tibial nerve is compressed. These conditions, often referred to as carpal tunnel syndrome and tarsal tunnel syndrome, respectively, frequently affect individuals who perform repetitive hand or foot movements.
Causes of Peripheral Nerve Damage
Peripheral nerve damage can stem from a multitude of causes, encompassing traumatic injuries, such as cuts, fractures, or dislocations. These injuries can directly damage the nerve fibers, leading to temporary or permanent impairments. Other causes include exposure to toxins, infections, or metabolic disorders.
Certain medical conditions, such as diabetes and autoimmune disorders, can also contribute to peripheral nerve damage. Chronic conditions like diabetes can cause nerve damage due to elevated blood sugar levels, which can impair blood flow to the nerves and lead to long-term complications.
Symptoms of Peripheral Nerve Issues
The symptoms associated with peripheral nerve problems are often diverse and can range from mild discomfort to severe debilitating pain. These symptoms often manifest as numbness, tingling, or burning sensations in the affected area. Pain can be described as sharp, shooting, or aching, and can vary in intensity. The location and type of symptoms can provide valuable clues to the specific nerve involved and the underlying cause.
Muscle weakness or atrophy (wasting) can also be present, potentially affecting the ability to perform everyday tasks. A progressive loss of sensation in the affected area is another common symptom, which can eventually impair the individual's ability to perceive touch, temperature, or pain.
Diagnosis and Evaluation
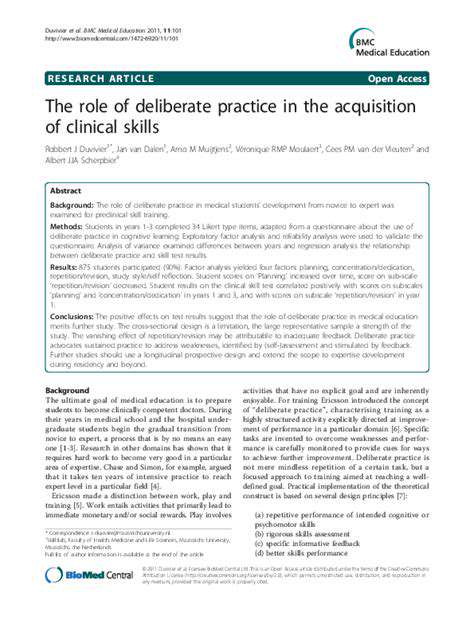
Diagnosing peripheral nerve issues often involves a comprehensive evaluation, combining a detailed medical history with a physical examination. The doctor will assess the patient's symptoms, including the location, duration, and characteristics of pain or other sensations. A detailed neurological examination focusing on reflexes, muscle strength, and sensation is crucial to pinpoint the affected nerve. This assessment helps to rule out other potential causes and guide further diagnostic tests, such as nerve conduction studies and electromyography (EMG).
Treatment Options for Peripheral Nerve Issues
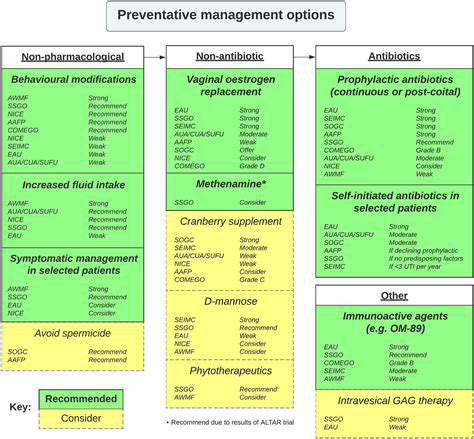
Treatment for peripheral nerve issues varies significantly depending on the underlying cause and severity of the condition. Conservative treatments, such as physical therapy, occupational therapy, and medications to manage pain and inflammation, are often the initial approach. Surgical intervention might be necessary in cases of severe nerve compression or when conservative treatments prove insufficient. The goal of treatment is to alleviate symptoms, restore nerve function, and improve the patient's overall quality of life.
Specific treatments may include splinting, bracing, or injections to reduce pressure on the affected nerve. Furthermore, lifestyle modifications, such as weight management and exercise, may play a crucial role in managing conditions like diabetic neuropathy.
Vascular Conditions: When Blood Flow is Compromised
Understanding Vascular Conditions
Vascular conditions encompass a wide range of diseases affecting the blood vessels throughout the body. These conditions can impact the arteries, veins, and capillaries, disrupting the normal flow of blood and potentially leading to serious health complications. Understanding the different types of vascular conditions is crucial for early detection and appropriate treatment. Early intervention can significantly improve outcomes.
Arterial Diseases: A Closer Look
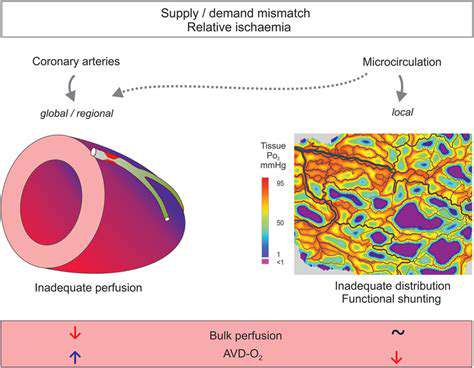
Arterial diseases, such as atherosclerosis, involve the hardening and narrowing of the arteries. This process, often caused by plaque buildup, restricts blood flow to vital organs and tissues. High cholesterol and high blood pressure are major risk factors for arterial diseases. Managing these risk factors through lifestyle changes and medication can significantly reduce the risk of developing these conditions.
Venous Disorders: Common Issues
Venous disorders, such as varicose veins and deep vein thrombosis (DVT), affect the veins. Varicose veins are characterized by enlarged, twisted veins, often appearing on the legs. DVT, a more serious condition, involves blood clots forming in the deep veins, potentially traveling to the lungs. Prompt diagnosis and treatment are essential for preventing complications from venous disorders. Seeking medical attention for any unusual leg pain or swelling is crucial.
Peripheral Artery Disease (PAD): Impact on Circulation
Peripheral artery disease (PAD) is a condition that affects the arteries in the limbs, particularly the legs and feet. It results in reduced blood flow to these extremities, causing symptoms such as pain, cramping, and numbness, especially during exercise. Early detection of PAD is crucial to prevent further progression and potential amputation. Lifestyle modifications, such as regular exercise and a healthy diet, can significantly improve outcomes in PAD management. Monitoring symptoms and consulting a doctor are essential.
Risk Factors for Vascular Conditions
Several factors contribute to the development of vascular conditions. These include high blood pressure, high cholesterol, smoking, diabetes, obesity, and a sedentary lifestyle. Maintaining a healthy weight, quitting smoking, and engaging in regular physical activity can reduce the risk of developing these conditions. A balanced diet rich in fruits, vegetables, and whole grains also plays a vital role in cardiovascular health.
Diagnosis and Treatment of Vascular Conditions
Diagnosing vascular conditions often involves a combination of physical examinations, medical history reviews, and diagnostic tests, such as ultrasound, angiography, and blood tests. Treatment options vary depending on the specific condition and its severity. These options may include lifestyle modifications, medications, and in some cases, surgical interventions. Working closely with a healthcare professional is essential for developing an effective treatment plan. Regular follow-ups are crucial for monitoring progress and adjusting treatment as needed.
Living with Vascular Conditions
Living with a vascular condition requires ongoing management and lifestyle adjustments. This may include adhering to prescribed medications, modifying dietary habits, and engaging in regular exercise. Managing risk factors and seeking support from healthcare providers are crucial for maintaining overall well-being. Support groups and educational resources can provide valuable information and guidance for individuals living with vascular conditions.
Trauma and Injuries: Physical Damage to the Hand
Fractures and Dislocations
Fractures, a common type of trauma to the hand, occur when a bone in the hand is broken. These breaks can range from hairline fractures, which are barely visible cracks, to complete breaks that result in the bone being shattered into multiple pieces. The severity of a fracture depends on the location and extent of the break, and can impact the hand's ability to function normally. Treatment for fractures typically involves immobilization with a cast or splint, and sometimes surgery to realign and stabilize the broken bone. Proper healing time varies, but often requires several weeks or even months of careful attention and rehabilitation.
Dislocations, another significant type of injury, involve the displacement of a joint in the hand. This happens when the end of one bone in a joint is forced out of its normal position relative to the other bone. Dislocations are often accompanied by pain, swelling, and significant instability in the affected joint. Prompt medical attention is crucial to reduce pain and prevent further damage. Treatment generally involves realignment of the joint, and often requires splinting or surgery, depending on the severity of the dislocation.
Soft Tissue Injuries
Soft tissue injuries encompass a wide range of damage to the hand's tendons, ligaments, muscles, and nerves. These injuries can result from blunt force trauma, cuts, or repetitive strain. A sprain, for example, occurs when a ligament is stretched or torn, while a strain involves damage to a muscle or tendon. The degree of injury can vary greatly, from minor discomfort to significant impairment of hand function. Immediate treatment for soft tissue injuries often involves rest, ice, compression, and elevation (RICE). More severe cases might necessitate physical therapy, pain management, or even surgical intervention to repair damaged tissues.
Nerve damage, a particularly concerning soft tissue injury in the hand, can result in numbness, tingling, or loss of sensation. Different types of nerve injuries require different levels of care. In some cases, the nerve may heal on its own, but in others, surgical intervention may be necessary to repair or restore the nerve's function. The symptoms and severity of the nerve damage will influence the treatment plan and recovery time.
Open Wounds and Infections
Open wounds, such as cuts, lacerations, and punctures, are another significant source of trauma to the hand. These wounds can expose underlying tissues and increase the risk of infection. Proper cleaning and disinfection of the wound are critical to preventing infection and promoting healing. Depending on the depth and severity of the wound, stitches or sutures may be required to close the skin and promote proper healing. The risk of infection is always a concern with open wounds, and prompt medical attention is essential to prevent complications.
Hand infections, if left untreated, can lead to severe complications, including permanent damage to the hand. Early diagnosis and appropriate antibiotic treatment are vital to combat infection. Prompt medical attention is crucial to limit the extent of the damage and prevent more serious consequences. Post-treatment care is equally important to prevent recurrence and ensure proper healing.
Careful attention to hand hygiene and wound care is vital in preventing infections. Prompt medical attention and appropriate treatment of open wounds are essential in preventing complications and ensuring optimal hand function.
Lifestyle Factors and Medications: Contributing Factors
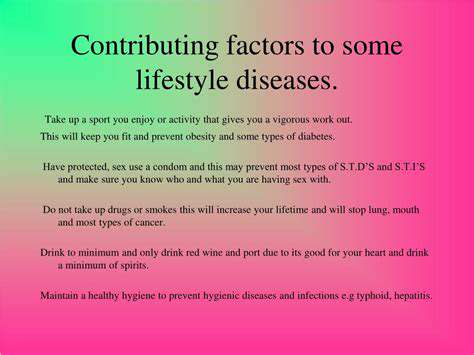
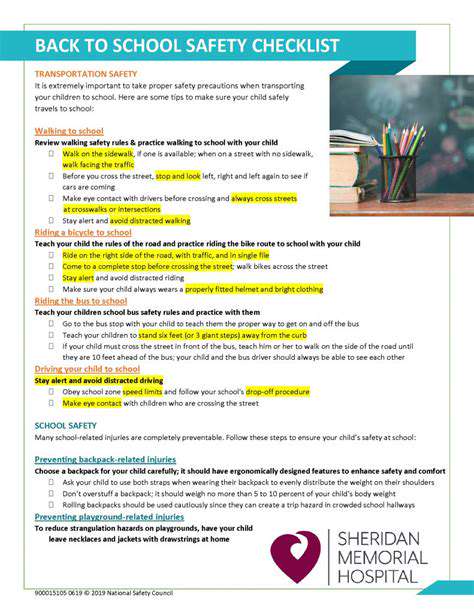
Lifestyle Modifications for Better Health
Adopting healthy lifestyle choices is crucial for overall well-being and can significantly impact the effectiveness of medications. A balanced diet rich in fruits, vegetables, and whole grains provides essential nutrients for optimal bodily function. Regular physical activity, such as brisk walking, jogging, or swimming, promotes cardiovascular health and helps manage weight, which is often a factor in many chronic conditions.
Getting enough quality sleep is also vital. Adequate rest allows the body to repair and rejuvenate, improving mood, concentration, and overall resilience to stress. Consistent sleep patterns, coupled with a relaxing bedtime routine, can greatly enhance the body's ability to cope with various health challenges.
Medication Adherence and Management
Taking medications as prescribed is paramount for achieving therapeutic benefits. This includes understanding the medication's purpose, dosage, and potential side effects. Regular communication with healthcare providers is essential to address any concerns or questions regarding medication use and to ensure the treatment plan is aligned with your specific needs. This open dialogue allows for adjustments to be made, if necessary, to optimize medication effectiveness and minimize potential risks.
Proper medication storage is also critical. Keeping medications in their original containers, away from direct sunlight and extreme temperatures, helps maintain their potency and effectiveness. Understanding the specific storage requirements for different medications is crucial for preserving their quality and avoiding potential harm.
Stress Management Techniques
Chronic stress can negatively impact both physical and mental health, potentially influencing medication effectiveness. Implementing stress-reduction techniques like meditation, deep breathing exercises, or yoga can help manage stress levels and promote overall well-being. Stress management techniques, if practiced consistently, can lead to a significant improvement in overall health and contribute to improved adherence to medication regimens.
Finding healthy ways to cope with stressful situations and daily pressures can improve your ability to manage your health conditions effectively. These techniques can also improve your ability to maintain a consistent medication schedule, which is an important factor in the effectiveness of medical interventions.
Nutrition and Dietary Considerations
Certain dietary components can either enhance or hinder the effectiveness of medications. For instance, some foods can interact with specific medications, potentially affecting their absorption or metabolism in the body. Understanding these interactions is critical for optimizing medication efficacy and preventing adverse effects. A registered dietitian or nutritionist can provide personalized guidance on dietary strategies that support medication management and overall health.
A balanced diet that provides essential vitamins, minerals, and antioxidants can bolster overall health and create a conducive environment for medications to function optimally. This includes focusing on nutrient-rich foods and limiting processed foods, sugary drinks, and excessive unhealthy fats.
The Role of Regular Check-ups
Regular check-ups with healthcare providers are essential for monitoring medication efficacy and potential side effects. These appointments allow for adjustments to treatment plans based on individual responses to medications. This proactive approach ensures that the medication regimen remains optimal and addresses any emerging health concerns promptly and effectively.
Regular monitoring also helps in identifying potential drug interactions or adverse effects that might not be immediately apparent. Proactive communication with your doctor during these check-ups allows for early intervention and adjustments to improve health outcomes.