Innovative Approaches for Athlete Hand Care
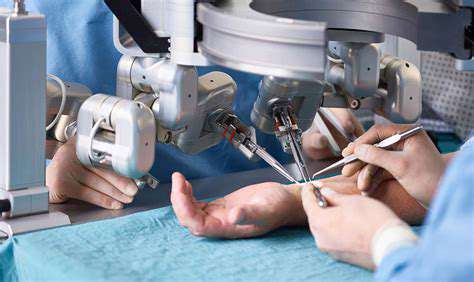
Soft Tissue Injury Evaluation
Not all wounds are equal. A superficial scrape differs vastly from a deep laceration near tendons. Doctors measure wound dimensions, check for foreign objects, and test underlying structure integrity. Severe soft tissue damage often requires microsurgery to preserve function, especially when tendons or ligaments are involved. The evaluation determines whether stitches suffice or if operating room intervention becomes necessary.
Fracture Assessment
X-rays reveal what eyes can't see—hairline fractures, bone fragments, or joint misalignments. A boxer's fractured metacarpal needs different management than a child's greenstick fracture. Fracture patterns dictate treatment: some heal with casting, others need surgical pins. Stability is key; unstable fractures may displace during healing, requiring more aggressive intervention.
Imaging Techniques and Interpretation
Modern imaging goes beyond basic X-rays. CT scans detail complex fractures, while MRIs visualize soft tissue damage like torn ligaments. Radiologists analyze these images like puzzles—a displaced bone fragment might indicate tendon entrapment. Accurate interpretation prevents overlooked injuries that could impair long-term function. For musicians or surgeons, even minor undiagnosed damage could end careers.
Personalized Training Regimens for Hand Strength and Endurance
Understanding Hand Strength and Endurance
Our hands perform miracles daily—from delicate embroidery to deadlifting weights. Customized training accounts for individual anatomy and goals, whether rehabilitating injuries or enhancing performance. A pianist needs different endurance than a rock climber. Understanding which muscles control grip versus fine movements allows targeted exercises that prevent overuse injuries.
Biomechanics matter. The flexor digitorum profundus muscle flexes fingertips differently than the lumbricals. Tailored programs adjust resistance based on these muscle interactions, ensuring balanced development without straining vulnerable structures like the A2 pulley in climbers.
Identifying Individual Needs and Goals
Before prescribing exercises, therapists assess baseline strength using dynamometers and pinch gauges. A baker recovering from carpal tunnel surgery has different needs than a gamer preventing repetitive strain. Clear objectives shape the regimen: perhaps improving jar-opening strength for elderly patients or enhancing pinch grip for jewelers. Lifestyle integration is crucial—a cashier's training differs from a drummer's.
Designing Effective Exercises
Variety prevents plateaus. Therapists might combine putty exercises for overall strength with bead-transfer tasks for dexterity. Progressive overload principles apply: gradually increasing resistance from 1lb to 5lbs over weeks. For arthritis patients, emphasis shifts to non-painful range-of-motion exercises that maintain joint mobility without exacerbating inflammation.
Progressive Overload and Adaptation
Muscles adapt to stress. Starting with 2-minute squeezes on a soft ball, patients advance to 5 minutes on firmer resistance. Rock climbers might hang from increasingly smaller ledges. The key? Systematic progression avoids overwhelming tissues while stimulating growth. Even small weekly increments—like adding 10 seconds to a static hold—yield measurable gains over months.
Monitoring Progress and Making Adjustments
Data drives adjustments. Monthly grip strength tests show trends; sudden drops may indicate overtraining. Patients log discomfort levels—a 3/10 pain during exercise might be acceptable, but persistent 5/10 signals needed modifications. This feedback loop keeps programs effective and safe, especially when recovering from injuries where pushing too hard risks regression.
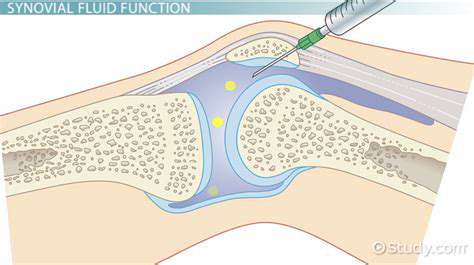
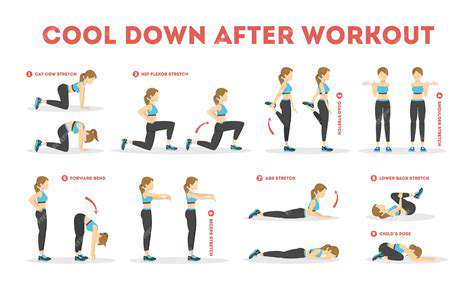
Safety Considerations and Precautions
Hands are fragile ecosystems of bones, nerves, and tendons. Warm-ups increase blood flow; contrast baths (hot/cold soaks) reduce post-exercise swelling. Proper form prevents common pitfalls like wrist flexion during grip training, which strains tendons. Those with conditions like rheumatoid arthritis require specially modified tools to avoid joint stress. Always consult hand specialists before starting intensive regimens.
The Role of Technology in Optimizing Athlete Hand Care
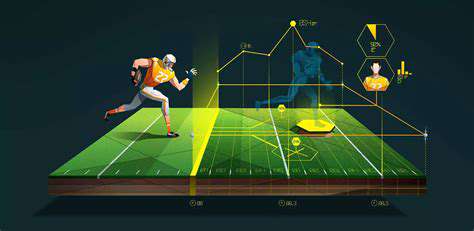
The Automation of Tasks
Gone are the days of manual therapy logs. AI-powered apps now track rehabilitation progress, adjusting exercises based on performance data. Sensors in grip tools measure force output, creating precise strength baselines. This automation reduces human error in tracking recovery milestones—critical when deciding when an NFL lineman can safely return to play.
Enhanced Communication and Collaboration
Cloud platforms unite athletes, coaches, and therapists. A quarterback's hand therapist in New York can monitor his grip strength readings in real-time from Texas. Shared digital dashboards ensure everyone stays aligned on recovery goals, preventing miscommunication that could delay return-to-play decisions. Video consultations bring specialists into rural areas lacking hand clinics.
Increased Efficiency and Productivity
Portable EMG devices identify muscle imbalances during specific motions—like a tennis serve—in minutes rather than requiring lab tests. This efficiency lets athletes correct biomechanical flaws before they cause injuries. Meanwhile, 3D-printed splints customized from MRI scans provide perfect fits faster than traditional casting methods.
Data-Driven Decision Making
Machine learning analyzes thousands of MLB pitcher hand injuries, identifying risk factors like specific grip angles. Teams now use these insights to modify training, reducing ulnar collateral ligament tears by 28% in one study. Wearables monitoring vibration exposure help construction workers avoid hand-arm vibration syndrome through timely breaks.
Improved Customer Experience
Virtual reality rehab transforms tedious exercises into engaging games—patients climb mountains by completing grip sequences. This gamification improves compliance, with studies showing 40% higher completion rates for tech-enhanced rehab. Apps provide real-time form feedback during home exercises via smartphone cameras, preventing incorrect movements that could hinder recovery.
Accessibility and Inclusivity
Voice-activated devices assist arthritis patients in tracking medication schedules. Affordable motion-capture gloves bring professional-grade biomechanical analysis to high school athletes. Such innovations democratize access to care that was once exclusive to elite performers, potentially preventing career-ending injuries in developing athletes who lack expensive medical support.