Innovative Approaches to Treating Hand Nerve Damage

The Role of Biomaterials and Bioengineering
Biomaterials in Hand Regeneration
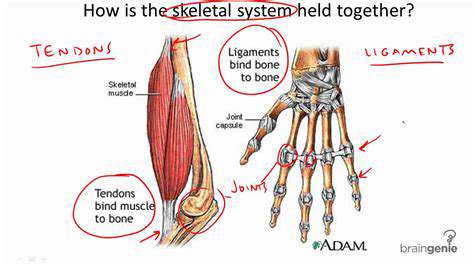
Biomaterials play a crucial role in hand regeneration by providing a scaffold for tissue growth and repair. These materials, carefully engineered to mimic the natural extracellular matrix, can act as temporary support structures, allowing cells to migrate, proliferate, and differentiate into functional tissues. This approach is particularly important in cases of severe hand trauma or congenital defects where native tissue may be insufficient or damaged beyond repair. The biocompatibility and biodegradability of these materials are paramount, ensuring they do not elicit an adverse immune response and gradually dissolve as the new tissue matures, leaving no foreign bodies behind. Precise control over the material's mechanical properties, such as strength and flexibility, is also vital to facilitate the restoration of normal hand function.
Different types of biomaterials, including polymers, ceramics, and composites, are being investigated for their potential in hand regeneration. Each material presents unique advantages and disadvantages in terms of bioactivity, degradation rate, and mechanical properties. Researchers are constantly working to optimize these materials, often incorporating bioactive molecules or growth factors to further enhance cell adhesion, proliferation, and differentiation. The future of hand regeneration likely hinges on the development of biomaterials that closely mimic the complex architecture and functionality of native hand tissues.
Bioengineering Approaches for Hand Functional Restoration
Bioengineering techniques go beyond simply providing a scaffold. They encompass a broader range of strategies focused on restoring the complex anatomy and physiology of the hand. This includes the development of techniques for tissue engineering, where cells are cultured and grown on biomaterials to create functional tissues. This approach has the potential to address a wide spectrum of hand injuries, from simple lacerations to complex amputations. Bioengineering also involves the design and fabrication of implantable devices that can help restore lost function, such as prosthetics with integrated sensors and actuators. These devices are designed to be intuitive and responsive, allowing users to regain a high degree of dexterity and control in their hands.
Advancements in 3D bioprinting are revolutionizing the field, allowing for the creation of highly customized scaffolds that precisely match the intricate anatomy of the hand. This technology enables the precise placement of cells and biomaterials, leading to more predictable and efficient tissue regeneration. The ability to tailor the bioprinted scaffolds to specific patient needs, considering factors like the extent of injury and the desired level of functional restoration, represents a significant step forward in the treatment of hand injuries.
Personalized Medicine in Hand Bioengineering
The application of personalized medicine is crucial in hand bioengineering, enabling the development of customized treatments tailored to the specific needs of each patient. This involves considering factors such as the patient's age, overall health, and the extent of the hand injury, which significantly impact the selection of biomaterials, tissue engineering approaches, and the design of prosthetic devices. This patient-specific approach aims to optimize the outcome of treatment, maximizing the likelihood of restoring optimal hand function and minimizing adverse events. Personalized therapies can incorporate genetic information to identify and target specific factors contributing to tissue repair and regeneration, leading to more effective and efficient treatment strategies.
Ethical Considerations in Biomaterial and Bioengineering Research
As biomaterials and bioengineering technologies continue to advance, ethical considerations surrounding their application in hand regeneration become increasingly important. Issues such as the potential for misuse, the equitable access to these advanced therapies, and the long-term effects on patient well-being must be carefully evaluated. Discussions regarding informed consent and the potential impact on patient autonomy in the context of experimental treatments are vital. Furthermore, the potential for bias in research design and the need for rigorous clinical trials to ensure safety and efficacy must be continually addressed. Ethical oversight and transparent communication are crucial to ensure that these innovative approaches are used responsibly and benefit patients while minimizing potential harm.