Therapies Aiding Finger Tendon Recovery
Introduction to Finger Tendon Injuries
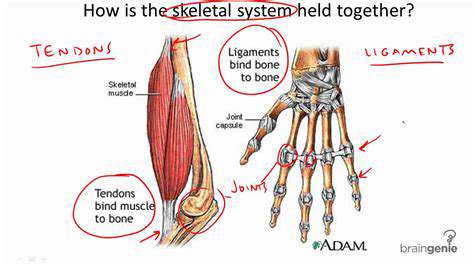
Understanding Finger Tendon Anatomy
Finger tendons act as biological cables, linking forearm muscles to delicate finger bones. These remarkable structures, woven from collagen fibers, empower everything from holding a pen to performing intricate surgical procedures. Their precise alignment determines whether we can button a shirt or play a concerto, making any disruption to this system potentially life-altering.
Multiple tendons work in perfect harmony - flexors bending fingers like marionette strings while extensors pull them straight. When this symphony falters, even simple tasks become frustrating challenges, underscoring why accurate injury assessment matters.
Common Causes of Finger Tendon Injuries
These injuries stem from diverse origins - office workers developing trigger finger from constant keyboard use, athletes snapping tendons during falls, or chefs suffering gradual wear from years of knife work. Repetitive strain creeps in silently, while traumatic injuries announce themselves with sudden pops and immediate dysfunction.
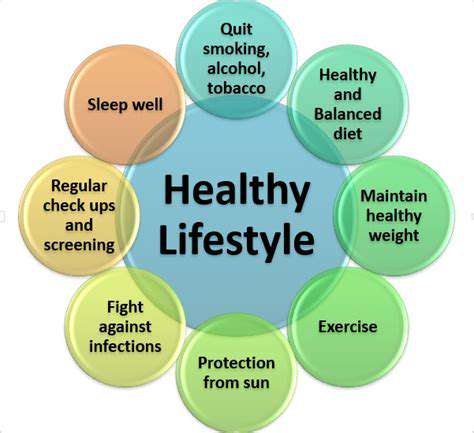
Systemic conditions add another layer of complexity - rheumatoid arthritis can erode tendons like termites in wood, while diabetes often impairs healing. Recognizing these hidden threats allows for earlier intervention and better outcomes.
Diagnosis and Evaluation of Finger Tendon Injuries
Skilled clinicians employ detective-like precision, combining physical exams with imaging tools. They'll trace pain patterns like cartographers mapping unknown territories, feeling for telltale gaps where tendons should be. Ultrasound becomes their x-ray vision, revealing torn fibers invisible to the naked eye.
Therapies for Finger Tendon Recovery
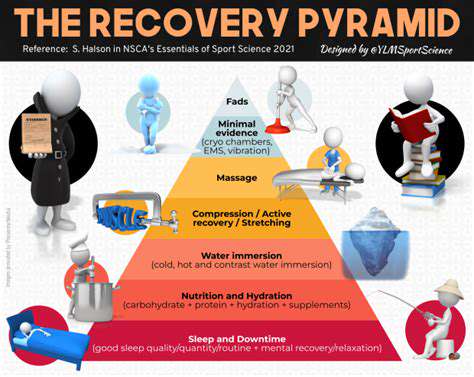
Treatment resembles a carefully choreographed dance - initial RICE protocol (Rest, Ice, Compression, Elevation) gives way to progressive rehabilitation. Specialized splints act as temporary scaffolds, protecting healing tissues while allowing controlled movement. For severe cases, microsurgery reconnects torn ends with sutures finer than human hair.
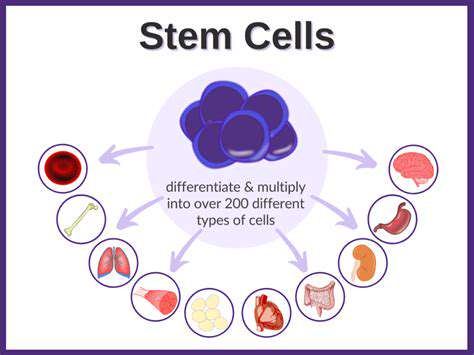
The recovery journey demands patience - tendons heal slower than bones, requiring months of guided therapy. Multidisciplinary teams become recovery architects, blending medical, therapeutic, and psychological support for optimal results.
Physical Therapy Techniques for Tendon Healing
Manual Therapy Techniques
Manual therapy represents the artful side of rehabilitation, where skilled hands detect subtle tissue restrictions invisible to machines. Therapists might use cross-friction massage to remodel scar tissue or gentle joint glides to restore fluid motion. These techniques often produce immediate improvements, like unlocking a stiff door with precisely applied pressure.
Different methods serve different purposes - myofascial release untangles connective tissue webs while strain-counterstrain techniques reset overactive muscle reflexes. The therapist's fingertips become diagnostic tools, reading tissue tension like Braille.
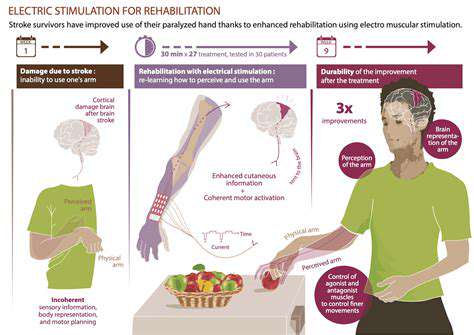
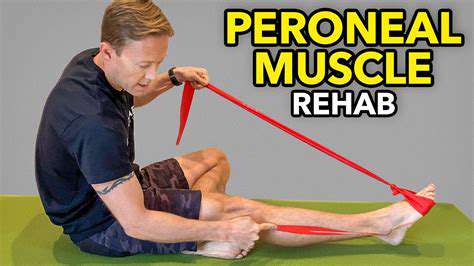
Exercise and Rehabilitation Protocols
Therapeutic exercises progress like a video game's difficulty levels - starting with simple tendon glides, advancing to resistance bands, eventually graduating to grip strengtheners. Each milestone represents regained independence, from holding a coffee cup to swinging a golf club.
Innovative tools enter the mix - putty for graded resistance, specialized dynamometers for precise strength measurement, even virtual reality systems making rehab engaging. The constant remains careful progression, never pushing beyond what healing tissues can tolerate.
Occupational Therapy and Adaptive Equipment
Occupational Therapy Approaches
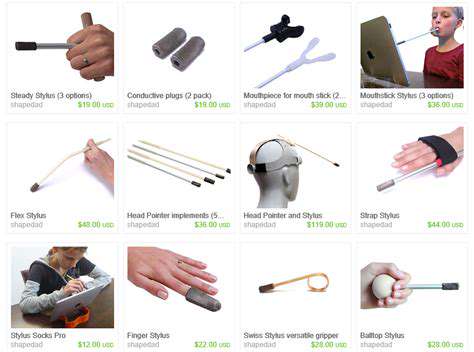
OT transforms limitations into possibilities, whether through customized splints or task modification strategies. The magic lies in personalized solutions - perhaps teaching a guitarist alternate fingerings or modifying kitchen tools for arthritic hands.
Adaptive Strategies and Assistive Technology
Innovation meets necessity - weighted utensils steady tremors, voice-activated devices bypass weak grips, and elastic shoelaces eliminate tying difficulties. The right adaptation can restore dignity along with function, whether it's a simple button hook or a high-tech prosthetic.
Role of Corticosteroids and Other Medications
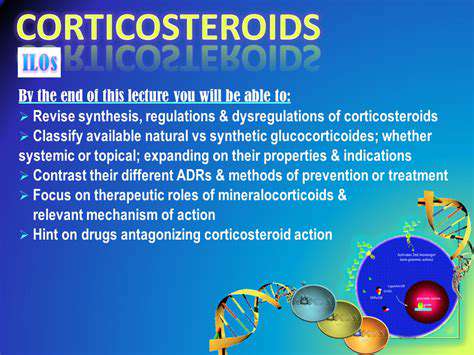
Corticosteroid Mechanism of Action
These biochemical firefighters work at the genetic level, suppressing inflammation's molecular alarms. They're the nuclear option when milder treatments fail, powerful but with significant collateral effects.
Impact on Inflammatory Mediators
Like turning down a raging storm to a drizzle, corticosteroids quiet cytokine storms that cause swelling and pain. This suppression comes at a cost - the body's natural defenses become muted, requiring careful risk-benefit analysis.
Alternative Anti-inflammatory Agents
The pharmaceutical toolbox keeps expanding - from traditional NSAIDs to cutting-edge biologics targeting specific inflammatory pathways. Choosing the right weapon depends on the inflammation's nature and intensity, like selecting the proper extinguisher for different fire types.