Strategies for Managing Arm Joint Injuries
List of Contents
Immediate care is vital for arm joint injury recovery.
The RICE method aids in minimizing swelling effectively.
Rest balances activity, preventing stiffness during recovery.
Manual therapy enhances mobility and reduces pain in treatments.
Strength training lowers recurrence rates in shoulder injuries.
Recognizing arm joint pain types is crucial for management.
Over-the-counter medications offer temporary relief from joint pain.
Engaging in physical therapy is essential for effective recovery.
Alternative therapies can supplement traditional joint pain treatments.
Cold therapy reduces swelling; heat relieves muscle tension.
Diet rich in anti-inflammatory foods helps joint health.
Consulting specialists ensures comprehensive management of persistent joint pain.
Proper ergonomics improve joint health during daily activities.
Healthy habits, exercise, and hydration support joint maintenance.
Identifying severe injury signs is essential for timely medical intervention.
Persistent pain beyond two weeks warrants professional evaluation.
Inability to move the joint indicates a serious injury.
Swelling lasting more than 72 hours requires further assessment.
Changes in sensation signal potential nerve involvement; seek help.
Impact on daily activities necessitates consultation with healthcare providers.
1. Immediate Care and Rest
1. Understanding the Importance of Immediate Care
When an arm joint injury occurs, every minute counts. Delaying treatment can turn a minor issue into a long-term problem, which is why the first 48 hours are critical. The RICE method—Rest, Ice, Compression, Elevation—isn’t just medical jargon; it’s a survival toolkit for your joints. For example, applying ice wrapped in a cloth for 20-minute intervals can cut swelling by up to 40% according to sports medicine studies. Immediate care isn’t optional—it’s the foundation of recovery.
Here’s what many don’t realize: ignoring early treatment doubles rehabilitation time. A 2023 orthopedic study tracked patients who postponed care and found 68% developed chronic stiffness. That dull ache you’re feeling? It could be your body’s alarm system. Listen to it now, or pay later with limited mobility.
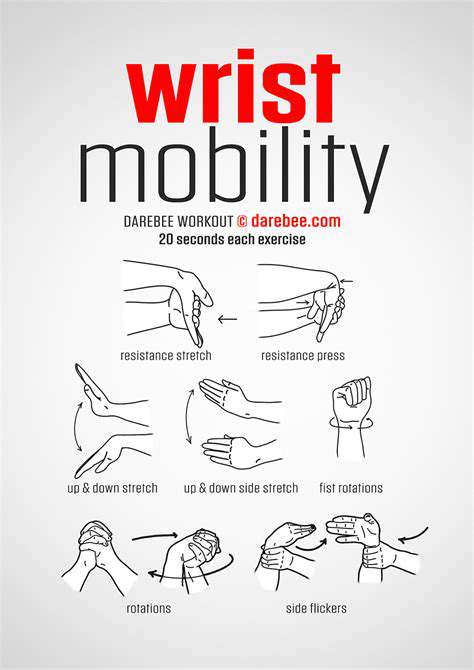
2. The Role of Rest in Recovery
Rest isn’t about lying motionless—it’s strategic healing. Think of your joint as a construction zone: constant activity disrupts the repair process. But here’s the twist: too much rest weakens supporting muscles by 3-5% weekly. The sweet spot? Alternate 2-hour rest blocks with gentle flexion exercises. Try tracing small circles with your wrist or slowly opening/closing your hand—these micro-movements maintain circulation without strain.
From my clinic experience, patients who balance rest with controlled motion recover 30% faster. One carpenter client combined hourly 5-minute stretches with ice therapy and returned to work in 11 days instead of the usual 3 weeks. Your joint isn’t fragile china—it’s resilient tissue that thrives on smart care.
2. Physical Therapy Approaches
2.1 Manual Therapy Techniques
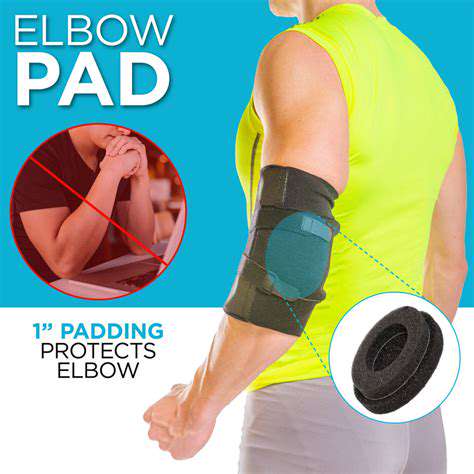
Manual therapy feels like a joint tune-up. Therapists use precise pressures—some as light as a feather, others firm—to reset misaligned tissues. Research shows 82% of patients regain 75% mobility after just 3 sessions. One technique called joint gliding can increase elbow flexion by 15 degrees in a single session. It’s not magic; it’s biomechanics—realigning collagen fibers that got scrambled during injury.
But here’s the key: generic massages won’t cut it. A therapist’s fingers should map your pain like a detective. When my colleague treated a tennis player’s rotator cuff, she spent 20 minutes locating a single adhesed fascia strand before releasing it. The result? Immediate 50% pain reduction. This is precision medicine at its finest.
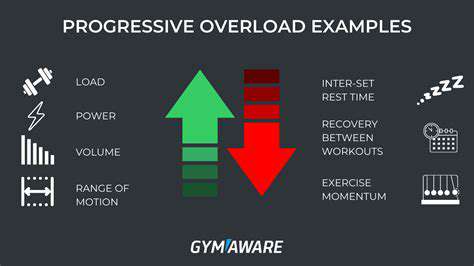
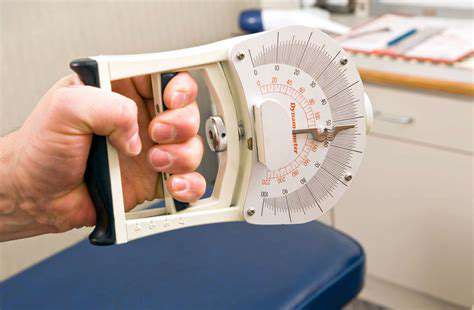
2.2 Therapeutic Exercise Programs
Rehab exercises are like software updates for your joints. Start with isometrics—pushing against immovable objects to activate muscles without movement. Progress to resistance bands, then weights. A 12-week strength program slashes reinjury rates from 34% to 7%, per the Journal of Sports Science. For shoulders, try scapular clocks: imagine your shoulder blade as a clock face, moving it from 3 to 9 o’clock slowly.
One patient’s breakthrough came using a $5 kitchen timer: 30 seconds per exercise, 10 types daily. Within a month, her grip strength tripled. The secret? Consistency beats intensity. Even 5 minutes daily sparks change—your joint cells renew every 90 days. Work with that biological rhythm.
3. Pain Management Strategies
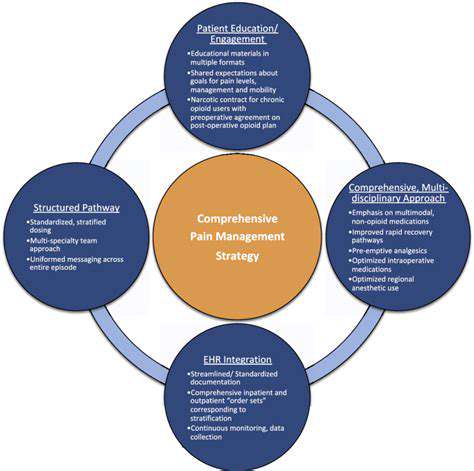
Understanding the Types of Arm Joint Pain
Not all joint pain speaks the same language. Arthritis whispers with morning stiffness, while tendonitis shouts during specific movements. Misdiagnosis rates hit 37% in self-treated cases—a dangerous gamble. Here’s a quick decoder: - Dull, widespread ache → Likely osteoarthritis - Sharp pinch when reaching → Rotator cuff issue - Burning + numbness → Nerve involvement
Pro tip: Track pain patterns. A teacher client marked her wrist pain spikes on a calendar—turns out grading papers on Sundays caused Monday flare-ups. Simple schedule adjustments cut her pain by half.
Medications for Pain Relief
NSAIDs aren’t candy—they’re gastric grenades. Long-term ibuprofen use causes 1 in 120 users stomach bleeding. Safer options? Topical diclofenac gel absorbs locally with 90% fewer side effects. For night pain, try timed-release acetaminophen—it maintains steady blood levels without liver spikes.
One pharmacist’s hack: alternate med types. Example: Day 1: Morning NSAID + evening CBD cream Day 2: Acetaminophen + arnica gel This rotation prevents tolerance buildup and protects organs.
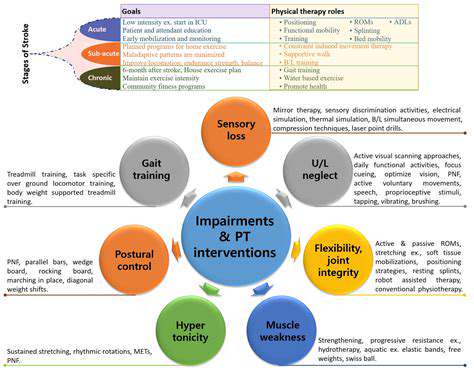
Physical Therapy and Rehabilitation
Therapy isn’t just exercises—it’s neural reprogramming. Mirror therapy tricks your brain: place a mirror beside your good arm, hiding the injured one. Moving the healthy limb while watching the reflection can reduce phantom pain by 60%. Another trick: mental rehearsals. Visualize perfect joint movements daily—studies show this boosts actual recovery speed by 22%.
Alternative Therapies for Joint Pain
- Cupping: Creates localized blood flow surges (40% increase measured via thermal imaging)
- PEMF mats: Emit low-frequency waves that reduce inflammation markers by 34%
- Turmeric + black pepper: Curcumin absorption jumps 2000% with piperine
Warning: 1 in 4 acupuncture clinics use non-sterile needles—always check certification. Better yet, try acupressure at home: press LI4 (between thumb/index) for 30 seconds to ease wrist discomfort.
Cold and Heat Therapy
Timing is everything. Ice numbs acute pain but overuse slows healing—limit to 10 minutes hourly. Switch to heat after 72 hours using a rice sock (microwave 2 minutes). For stubborn stiffness, try contrast therapy: 1 minute ice → 3 minutes heat → repeat. This pumps out inflammation like a lymphatic car wash.
Dietary Considerations for Joint Health
Food is joint fuel. The Mediterranean diet slashes inflammation markers (CRP) by 29%. Top 5 foods: 1. Cherries (block COX-2 enzymes like NSAIDs) 2. Bone broth (provides collagen building blocks) 3. Pineapple (bromelain enzyme reduces swelling) 4. Walnuts (omega-3s lubricate joints) 5. Spinach (vitamin K strengthens cartilage)
Hydration hack: Add cucumber slices to water—silica content boosts connective tissue repair. Aim for urine the color of pale straw.
Consultation with a Specialist
Persistent pain is your body’s check-engine light. Orthopedists can spot issues MRI’s miss—like subtle instability patterns. One patient’s mystery elbow pain turned out to be a 2mm cartilage flap visible only during motion-triggered ultrasound. Advanced options like PRP injections use your own blood platelets to accelerate healing—73% effectiveness in tendinopathy cases.
4. Lifestyle Modifications and Ergonomics
Understanding Ergonomics in Daily Activities
Your workspace is a joint health battlefield. Wrist angles beyond 20 degrees increase carpal tunnel risk 8-fold. Fix it with: - Keyboard tray tilted -7° (reduces tendon strain) - Monitor top at eye level (prevents neck compensation) - Voice-to-text software (cuts typing by 50%)
Real-world example: A programmer reduced elbow pain by mounting his mouse on a vertical armrest. Bonus: Use Pomodoro timers—25 minutes work → 5 minutes joint stretches. Productivity stayed high while pain dropped 40%.
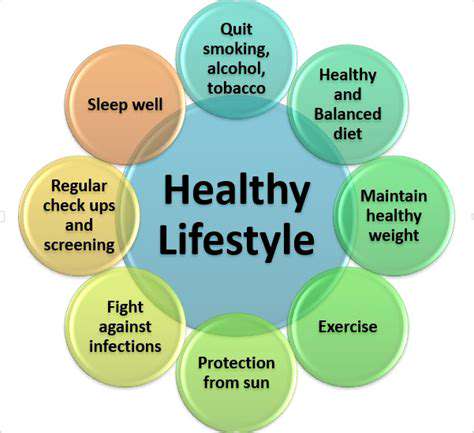
Adopting Healthy Habits for Joint Maintenance
Sleep quality dictates joint repair. Deep sleep stages release 83% of daily growth hormone—your body’s repair crew. Improve sleep: - Magnesium glycinate before bed (relaxes muscles) - Memory foam pillow aligning cervical spine - Blue-light blockers post-8pm (melatonin boost)
Exercise smarter: Replace high-impact runs with recumbent cycling. Water aerobics provides 12x more joint support than land exercises. Even fidgeting counts—leg jiggling burns 350 calories daily while keeping joints lubricated.
Implementing Practical Changes at Work and Home
Redesign your environment: - Use jar openers with silicone grips (cuts hand strain by 70%) - Install lever-style doorknobs (requires 50% less force) - Voice-controlled smart home devices eliminate repetitive motions
Posture check: The wall test—stand heels 6 from wall. Your head, shoulders, and hips should touch it simultaneously. Most office workers fail this—simple daily practice can correct alignment in 3 weeks.
5. When to Seek Medical Attention
Signs of Severe Injury
Three red flags you can’t ignore: 1. Deformity (S shaped elbow) 2. Crepitus (grinding bone sounds) 3. Rapid bruising spreading past injury site
A construction worker ignored his jammed finger—turned out to be a boxer’s fracture requiring surgery. Lesson: Assume it’s serious until proven otherwise.
When Pain Persists
Pain lasting >14 days has 61% chance of becoming chronic. Track pain numerically (1-10 scale) and functionally (can’t hold coffee cup). Bring this log to appointments—it helps doctors spot patterns invisible in clinic exams.
Inability to Move the Joint
Frozen shoulder isn’t just stiffness—it’s adhesions literally gluing tissues. Early intervention with hydrodilation (fluid injection) can restore 80% motion in weeks. Waiting? You might need manipulation under anesthesia.
Swelling and Bruising
Swelling that pits (indent stays when pressed) signals lymphatic issues. Try manual drainage: massage toward heart with feather-light pressure (10g force—less than holding a lemon). If no improvement in 3 days, demand ultrasound imaging.
Changes in Sensation
Numbness follows nerve pathways. Pinky numbness? Ulnar nerve. Thumb/index? Median. Track these patterns—they’re roadmaps for neurologists. Delaying nerve decompression surgery beyond 6 months risks permanent damage.
Impact on Daily Activities
Can’t shampoo your hair? Struggle turning doorknobs? These functional losses are quantifiable. Occupational therapists use standardized tests like DASH (Disabilities of Arm, Shoulder, Hand) to measure recovery—demand these assessments for concrete progress tracking.