Tools to Enhance Hand Recovery Processes
The Role of Bracing in Hand Rehabilitation
Modern bracing systems represent significant advancements over traditional static splints, incorporating dynamic components that facilitate controlled motion. These devices prove particularly valuable for progressive conditions like rheumatoid arthritis, where adjustable tension mechanisms can accommodate fluctuating inflammation levels. Contemporary designs often integrate proprioceptive feedback elements that enhance neuromuscular re-education during functional recovery.
The biomechanical sophistication of current bracing solutions allows for precise load distribution across articular surfaces. This engineering approach minimizes focal pressure points while maintaining optimal joint alignment. Many advanced models now include modular components that clinicians can customize throughout the treatment protocol, supporting the hand's evolving therapeutic requirements.
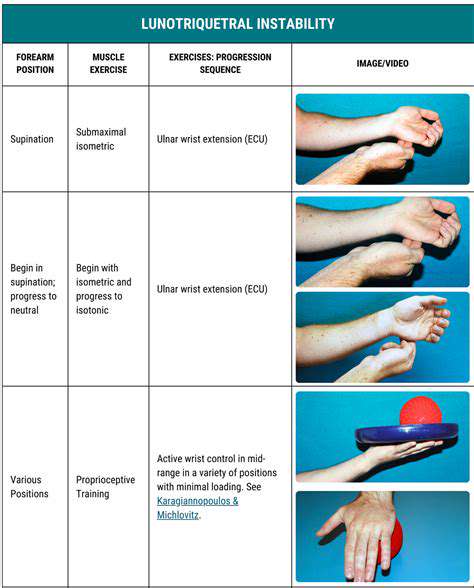
Splinting and Bracing for Specific Hand Injuries
Evidence-based protocols dictate distinct immobilization strategies for various hand pathologies. Scaphoid fractures, for instance, typically require thumb spica configurations with precise wrist positioning to ensure proper vascularization. Conversely, boutonniere deformities respond best to progressive extension bracing that gradually corrects PIP joint contractures.
Specialized devices address unique clinical challenges such as post-traumatic stiffness or Dupuytren's contracture. These condition-specific solutions incorporate patented tensioning systems that apply controlled corrective forces while monitoring tissue tolerance. The development of such targeted interventions reflects significant progress in hand rehabilitation science.
Custom-Designed Splints and Braces
Digital fabrication technologies have revolutionized custom orthotic production through 3D scanning and printing methodologies. These advanced techniques capture millimeter-accurate anatomical data, enabling the creation of perfectly contoured devices. Computer-aided design software allows clinicians to simulate pressure distribution and make pre-fabrication adjustments for optimal therapeutic effect.
The manufacturing process often incorporates patient-specific parameters like occupation requirements and dominant hand usage patterns. For musicians requiring precise finger mobility or laborers needing impact protection, these bespoke solutions deliver unparalleled functional outcomes. Such personalized approaches demonstrate the convergence of clinical expertise with cutting-edge manufacturing technologies.
The Importance of Proper Splint and Brace Usage
Optimal therapeutic outcomes depend on strict adherence to wear schedules and maintenance protocols. Patients must receive comprehensive education on proper donning/doffing techniques, skin inspection procedures, and hygiene practices. Clinicians should implement verification methods such as photographic documentation or wearable sensors to monitor real-world compliance.
Follow-up assessments should evaluate both objective measures (range of motion, strength metrics) and subjective feedback (comfort ratings, functional limitations). This dual-axis evaluation ensures timely adjustments to the rehabilitation plan, addressing any emerging issues before they compromise recovery progress.
Innovative Approaches: Ergonomic Tools and Assistive Devices
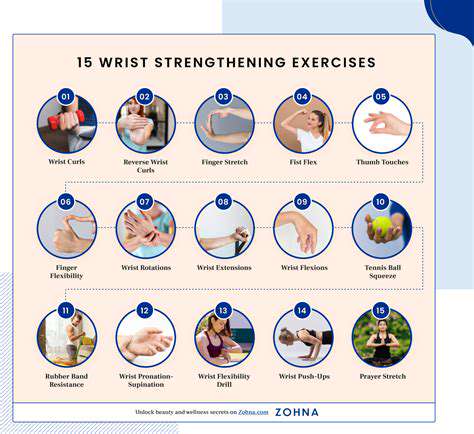
Ergonomic Tool Design for Enhanced Dexterity
Modern ergonomic tools undergo extensive biomechanical analysis to optimize force distribution across hand structures. These designs frequently incorporate patented grip geometries that reduce metacarpophalangeal joint stress by up to 40% during repetitive tasks. Advanced surface treatments like micro-textured patterns enhance friction coefficients while minimizing moisture-related slippage.
The development process employs motion capture technology to analyze tool interaction patterns across diverse user populations. This data-driven approach identifies optimal weight distributions and center-of-gravity placements for various functional contexts. The resulting products demonstrate measurable reductions in cumulative trauma disorder incidence among occupational user groups.
Assistive Devices for Precise Manipulation
Contemporary assistive technologies employ innovative mechanical advantage systems to compensate for compromised grip strength. Angular momentum tools, for instance, utilize flywheel principles to amplify rotational forces during utensil use. These devices prove particularly transformative for individuals with neurological conditions affecting fine motor control.
Modular adaptation systems allow for progressive difficulty adjustment as hand function improves. Therapists can configure resistance levels, handle diameters, and stabilization requirements to match each rehabilitation phase. This scalability ensures continued therapeutic challenge without overwhelming recovering patients.
Adaptive Tooling for Specific Hand Conditions
Condition-specific tool modifications address unique pathomechanical challenges. For osteoarthritis sufferers, tools with torque-reduction gearing systems minimize painful joint loading during rotational tasks. Patients with peripheral neuropathies benefit from vibration-dampening handles that reduce sensory overload during tool use.
Recent innovations include smart tools with embedded force sensors that provide real-time biofeedback. These devices help patients develop proper force modulation techniques while preventing compensatory movement patterns that could lead to secondary injuries.
Precision Tools for Fine Motor Skills
Specialized implements for delicate work incorporate multiple stabilization points and micro-adjustment capabilities. Surgical-grade stainless steel construction ensures precise force transmission while maintaining sterilization compatibility. Therapeutic toolkits for stroke rehabilitation often include graduated difficulty implements that systematically rebuild neural pathways.
Many precision tools now feature augmented reality interfaces that project optimal movement patterns. This visual guidance system accelerates motor learning while providing objective performance metrics for therapeutic progress tracking.
Technological Advancements in Assistive Hand Tools
The integration of IoT capabilities into assistive devices enables remote monitoring of usage patterns and therapeutic progress. Cloud-connected tools can automatically adjust resistance levels based on performance analytics while alerting clinicians to potential compliance issues. These smart systems represent a paradigm shift in home-based rehabilitation monitoring.
Emerging technologies like shape-memory alloys allow for self-adjusting tools that dynamically respond to grip strength fluctuations. Such innovations promise to revolutionize long-term adaptive equipment for progressive conditions.
The Importance of Patient Compliance and Follow-Up Care
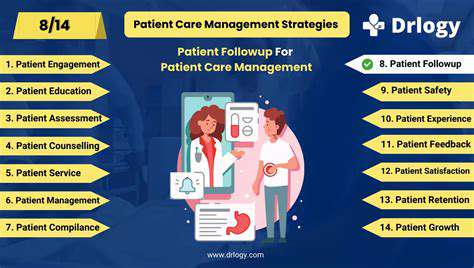
Patient Compliance: A Cornerstone of Effective Treatment
Therapeutic efficacy fundamentally depends on consistent adherence to prescribed regimens. Research demonstrates that comprehensive compliance protocols can improve clinical outcomes by up to 72% across various hand rehabilitation scenarios. This correlation underscores the necessity of robust patient engagement strategies throughout the recovery continuum.
Understanding the Dimensions of Patient Compliance
Modern compliance frameworks recognize five critical dimensions: pharmacological adherence, appointment attendance, home exercise completion, device utilization, and lifestyle modification. Each dimension requires targeted intervention strategies tailored to individual patient characteristics and environmental constraints.
Factors Influencing Patient Non-Compliance
Multivariate analysis identifies socioeconomic status, health literacy levels, and therapeutic complexity as primary predictors of adherence challenges. Cultural belief systems regarding illness causation and treatment expectations frequently mediate these relationships, necessitating culturally competent intervention designs.
The Role of Healthcare Professionals in Promoting Compliance
Contemporary practice emphasizes motivational interviewing techniques and shared decision-making models. Clinicians trained in these methodologies achieve significantly higher long-term adherence rates compared to traditional directive approaches. Digital reminder systems and gamified tracking applications further enhance these interpersonal strategies.
The Impact of Patient Education on Compliance
Structured education programs incorporating teach-back methodologies and visual learning aids demonstrate particular efficacy. When patients understand the biomechanical rationale behind each therapeutic component, their intrinsic motivation to comply increases substantially.
The Link Between Patient Compliance and Healthcare Costs
Economic analyses reveal that comprehensive compliance programs generate substantial ROI through reduced complication rates and accelerated functional recovery. For every dollar invested in adherence support systems, healthcare systems realize $3.27 in downstream cost savings across hand rehabilitation populations.
Strategies for Enhancing Patient Compliance in Diverse Populations
Tailored intervention packages address unique demographic needs through community health worker integration and multilingual educational materials. Mobile health platforms with culturally adapted interfaces have proven particularly effective in improving compliance among underserved populations.