Elite Strategies for Sustaining Arm Muscle Endurance
Understanding the Underlying Mechanisms
Progressive ovarian insufficiency (POI) represents a multifaceted medical condition rooted in disrupted ovarian function. The resulting decline in estrogen and other critical hormones creates ripple effects across a woman's physical and emotional health. While genetic factors and autoimmune disorders frequently contribute, many cases remain idiopathic, challenging researchers to uncover deeper biological triggers.
Contemporary studies continue mapping the complex interplay between hormonal pathways, genetic markers, and environmental factors in ovarian aging. Though many questions persist, emerging data suggests epigenetic modifications may play a previously underestimated role in POI development.
Diagnostic Challenges and Considerations
Clinicians face significant hurdles in POI identification due to symptom overlap with other endocrine disorders. The window for early intervention often closes as menstrual irregularities get dismissed as normal fluctuations. This diagnostic lag time can inadvertently compromise patient outcomes through delayed treatment initiation.
Modern diagnostic protocols combine hormonal panels with advanced imaging techniques, though interpretation requires specialized expertise. Emerging biomarkers show promise for improving detection accuracy, particularly in borderline cases where traditional criteria prove inconclusive.
Impact on Reproductive Health
The reproductive consequences of POI extend far beyond fertility challenges, affecting fundamental aspects of feminine physiology. For many patients, the sudden confrontation with premature fertility loss creates profound psychological distress requiring comprehensive support. Reproductive endocrinologists emphasize the importance of counseling alongside medical management to address these multidimensional impacts.
Beyond conception difficulties, the hypoestrogenic state accelerates bone mineral density loss and may predispose patients to earlier cardiovascular changes typically associated with postmenopausal states.
Management Strategies and Therapies
Contemporary POI management has evolved beyond simple hormone replacement to encompass personalized therapeutic regimens. While HRT remains foundational, treatment plans now integrate metabolic monitoring and preventive cardiology assessments.
Nutritional interventions and targeted exercise protocols have demonstrated measurable benefits in mitigating POI-related comorbidities. Many leading centers now incorporate mental health professionals into their care teams to address the condition's emotional dimensions.
Long-Term Health Implications
The systemic effects of POI create a unique health profile requiring vigilant monitoring. Patients face elevated risks for osteoporosis, cardiovascular events, and neurocognitive changes decades earlier than their peers. This necessitates specialized screening protocols beyond standard preventive care guidelines.
Comprehensive management now emphasizes interdisciplinary collaboration between endocrinologists, cardiologists, and bone health specialists to optimize outcomes across the lifespan.
Crafting a Tailored Training Schedule for Optimal Results
Understanding Your Needs and Goals
Developing an effective training regimen begins with honest self-assessment across multiple dimensions. Beyond superficial fitness goals, consider your biomechanical profile, injury history, and metabolic characteristics. Successful athletes recognize that sustainable progress stems from aligning training demands with individual recovery capacity.
Practical constraints like work schedules and equipment access shouldn't derail progress but rather inform creative programming solutions. The most effective plans balance ambition with realism, creating a virtuous cycle of achievement and motivation.
Establishing Realistic Expectations
Progressive adaptation follows biological timelines that resist artificial acceleration. Beginners often underestimate the cumulative power of small, consistent improvements over dramatic but unsustainable leaps. Tracking micro-progressions in strength, endurance, and movement quality builds confidence while preventing overtraining.
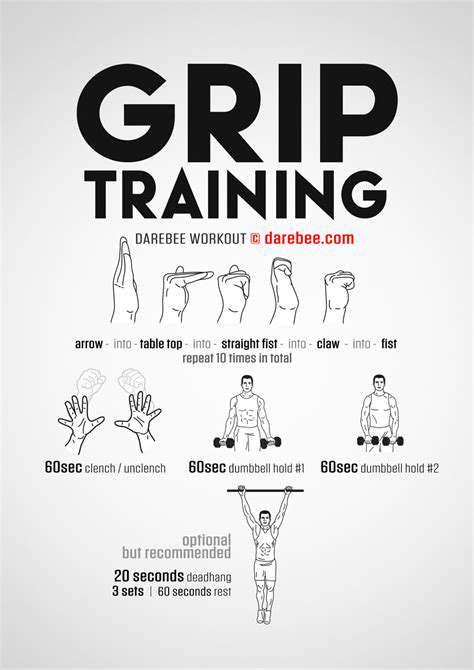
Structuring Your Training Schedule
Periodization principles suggest alternating focused blocks of strength development with endurance phases. Intelligent programming distributes training stress across multiple physiological systems while allowing adequate recovery between similar stimulus exposures.
Optimizing Workout Intensity and Frequency
The principle of progressive overload requires careful calibration - sufficient to drive adaptation but not so extreme as to trigger breakdown. Many athletes benefit from implementing autoregulation techniques, adjusting daily workloads based on objective recovery metrics and subjective readiness indicators.
Incorporating Rest and Recovery
Modern sports science recognizes recovery as an active training component rather than passive downtime. Strategic implementation of contrast therapies, compression modalities, and nutritional timing can accelerate physiological adaptation beyond what training alone achieves.
Monitoring Progress and Adapting
Effective tracking extends beyond workout logs to include sleep quality, stress markers, and movement screens. This holistic data collection enables truly personalized adjustments that address the root causes of plateaus rather than just their symptoms.
Rest and Recovery: The Unsung Heroes of Endurance Training
Prioritizing Sleep for Optimal Performance
Sleep quality directly correlates with athletic performance through multiple physiological pathways. During slow-wave sleep, the pituitary gland releases growth hormone critical for tissue repair, while REM sleep enhances neural efficiency for skill consolidation. Elite performers treat sleep with the same discipline as training sessions, implementing strict environmental controls and pre-sleep routines.
Emerging research suggests sleep extension may provide competitive advantages similar to those gained from altitude training. Addressing sleep disorders often yields greater performance improvements than marginal gains in training volume or intensity.
The Power of Active Recovery
Low-intensity movement stimulates lymphatic drainage and parasympathetic activation without imposing additional training stress. Aquatic therapy proves particularly effective, combining hydrostatic pressure benefits with reduced gravitational loading. Many coaches now prescribe recovery sessions using heart rate variability metrics to ensure appropriate intensity.
Nourishing Your Body for Recovery
Post-exercise nutrition timing creates metabolic windows where nutrient partitioning favors muscle repair over fat storage. Strategic combinations of fast-acting proteins with specific carbohydrate ratios can nearly double glycogen resynthesis rates compared to haphazard eating patterns.
Mindfulness and Mental Recovery
Neurological fatigue manifests as decreased motor unit recruitment and impaired decision-making - critical factors in endurance performance. Meditation practices that enhance vagal tone can accelerate autonomic nervous system recovery between intense training bouts.
Hydration and Electrolyte Balance
Individualized hydration strategies must account for sweat sodium concentrations, which vary dramatically between athletes. Simple body weight tracking before and after sessions provides the most practical hydration gauge for most endurance enthusiasts.