Understanding the Healing Process of Bone Fractures in Hands
The Initial Stages of Fracture Healing in the Hand
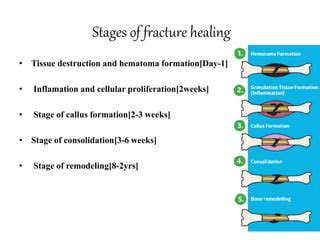
Initial Stages of Crack Nucleation
The initial stages of fracture often begin with the formation of tiny cracks, or flaws, within a material. These flaws, which can arise from various sources, such as manufacturing defects, material imperfections, or environmental degradation, are often microscopic and difficult to detect. Understanding the mechanisms that lead to the initiation of these cracks is crucial in predicting and preventing material failure.
These microscopic cracks act as stress concentrators, meaning they significantly amplify the stress within the material surrounding them. This localized stress intensification can eventually lead to crack propagation, a process that can rapidly escalate and result in catastrophic failure if not controlled.
Crack Propagation Mechanisms
Once a crack has nucleated, it begins to propagate through the material. This propagation can occur through various mechanisms, depending on the material's properties and the applied stress conditions. Understanding these mechanisms, such as fatigue, creep, and brittle fracture, is critical for designing structures that can withstand expected loads and stresses without failure.
One key mechanism is fatigue, a phenomenon that occurs when a material is subjected to repeated stress cycles. Over time, these cycles can cause microscopic cracks to grow and eventually propagate, leading to fracture. Another critical mechanism is creep, which involves the gradual deformation of a material under sustained stress over time. This can also contribute to crack growth, especially at elevated temperatures.
Material Properties and Fracture Toughness
The susceptibility of a material to fracture is significantly influenced by its inherent material properties. Factors such as the material's microstructure, grain size, and composition can all play a role in determining the material's resistance to crack propagation. Understanding the relationship between material properties and fracture behavior is essential for selecting appropriate materials for specific applications.
Fracture toughness, a material property that quantifies a material's resistance to crack propagation, is a crucial parameter in assessing the potential for fracture. Higher fracture toughness values generally indicate a greater resistance to crack growth and thus a higher safety margin.
Environmental Factors and Fracture
Environmental factors can significantly impact the rate of crack propagation. Exposure to corrosive environments, high temperatures, or other detrimental conditions can accelerate the degradation of materials and increase their susceptibility to fracture. For example, the presence of moisture or specific chemicals can lead to the formation of stress corrosion cracks, which can propagate rapidly and lead to unexpected failures.
Understanding the influence of these environmental factors is crucial for designing structures that can endure the expected operating conditions. Proper material selection and protective coatings can help mitigate the negative impact of environmental factors on fracture behavior.
The Role of Inflammation and Cellular Response
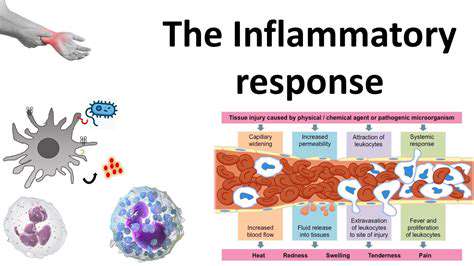
The Inflammatory Response
Inflammation, a fundamental biological response, is a complex process triggered by various stimuli, including infections, injuries, and immune responses. This response is crucial for protecting the body from harmful agents and initiating the healing process. Understanding the intricacies of inflammation is essential for comprehending numerous diseases and developing effective treatments. Inflammation involves a cascade of events, from the initial recognition of a threat to the eventual resolution of the inflammatory reaction, and it's not simply a binary on/off switch.
The key players in inflammation are specialized immune cells, such as macrophages and neutrophils, which release signaling molecules called cytokines. These cytokines orchestrate the inflammatory response by recruiting other immune cells to the site of injury or infection, increasing blood flow to the area, and promoting the repair of damaged tissues. The delicate balance of pro-inflammatory and anti-inflammatory mediators is vital for maintaining homeostasis and preventing excessive tissue damage.
Cellular Components in Inflammation
Several types of cells play critical roles in the inflammatory response. Macrophages, a type of white blood cell, are crucial for recognizing pathogens and initiating the inflammatory cascade. They engulf and destroy pathogens, and produce cytokines, signaling molecules that regulate the inflammatory response.
Neutrophils, another essential type of white blood cell, are the first responders to infection or injury. They migrate to the affected area and eliminate pathogens through phagocytosis, a process of engulfing and destroying foreign particles. The coordinated action of these cells, alongside other immune components, is essential for effectively combating harmful invaders and initiating tissue repair.
Inflammation and Disease
Chronic inflammation is a key contributor to many diseases, from cardiovascular disease to autoimmune disorders and certain types of cancer. Chronic inflammation can lead to persistent tissue damage and dysfunction, impacting organ systems and overall health. Understanding the mechanisms underlying chronic inflammation is essential for developing targeted therapies to mitigate its harmful effects.
For example, persistent inflammation in the arteries can contribute to the development of atherosclerosis, a condition that narrows and hardens blood vessels, increasing the risk of heart attacks and strokes. In autoimmune diseases, the body's immune system mistakenly attacks healthy tissues, leading to chronic inflammation and organ damage.
The Resolution of Inflammation
The inflammatory response, while crucial for protection, must eventually resolve to allow for proper tissue repair and healing. The resolution phase involves a shift from pro-inflammatory mediators to anti-inflammatory mediators, promoting tissue regeneration and repair. This transition is tightly regulated and involves specific signaling pathways that ensure the termination of the inflammatory response.
Dysregulation of the resolution phase can lead to persistent inflammation, contributing to chronic diseases. This makes the intricate process of resolving inflammation a critical area of research, with the potential to develop novel therapeutic strategies for managing and preventing chronic inflammatory diseases.
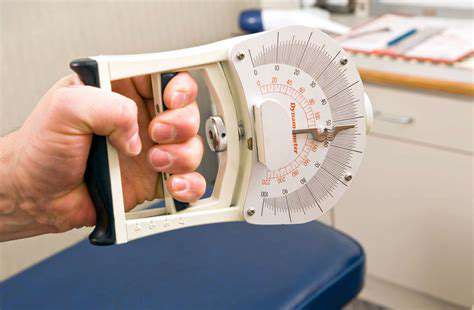
Factors Affecting Hand Fracture Healing Time
Patient Factors Affecting Healing Time
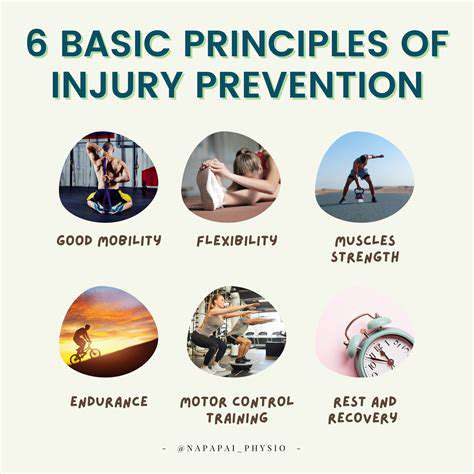
Patient age plays a significant role in the healing process. Younger patients generally exhibit faster bone regeneration due to their higher metabolic rate and increased cellular activity. Older individuals, however, may experience slower healing times due to decreased bone density and reduced blood flow, which are common age-related changes. Underlying health conditions, such as diabetes or osteoporosis, can also significantly impact the healing process, potentially leading to prolonged recovery times and increased risk of complications.
Furthermore, the patient's overall health and nutritional status are crucial. A balanced diet rich in essential nutrients, including calcium and vitamin D, is vital for optimal bone health and accelerates the healing process. Malnutrition or deficiencies in these key nutrients can hinder the body's ability to repair damaged tissue, leading to delayed healing and potential complications. Maintaining a healthy weight is also important, as excessive weight can put extra stress on the healing fracture site.
Severity of the Fracture
The severity of the fracture directly impacts the healing time. A simple fracture, characterized by a clean break with minimal displacement of bone fragments, often heals more quickly than a complex fracture. Complex fractures, involving multiple fragments, comminution (shattering of the bone), or displacement, may require more extensive treatment and a longer recovery period. The precise location of the fracture within the hand also influences the healing process, affecting the availability of blood supply to the affected area.
Type of Treatment
The chosen treatment method significantly impacts the healing time. Non-surgical interventions, such as casts or splints, are often used for less severe fractures. Surgical interventions, such as open reduction and internal fixation (ORIF), are frequently required for complex fractures. The complexity of the surgical procedure, the skill of the surgeon, and the quality of the implants used can all contribute to the overall healing timeline.
Fracture Location and Alignment
The location of the fracture within the hand significantly affects the healing process. Fractures in areas with abundant blood supply tend to heal faster than those in areas with limited blood flow. Proper alignment of the fractured bone fragments is crucial for optimal healing. Misalignment can lead to complications, such as malunion (improper healing) or nonunion (failure of the bone to heal), both of which can prolong the recovery period and potentially require additional interventions.
Immobilization Period and Compliance
The duration of immobilization, whether through casts, splints, or other devices, is a key factor in healing time. Following the prescribed immobilization period meticulously is essential for allowing the bone to heal properly. Failure to adhere to the prescribed immobilization period can result in delayed healing or complications, increasing the overall recovery time. Furthermore, the patient's willingness to comply with post-operative instructions and attend follow-up appointments is also crucial for successful healing.
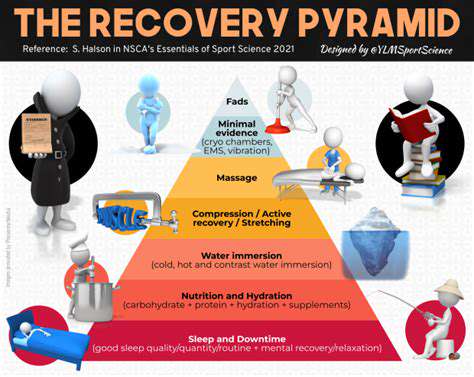
The Role of Physical Therapy
Post-fracture physical therapy plays a vital role in restoring hand function and accelerating the healing process. Early and appropriate physical therapy exercises help maintain joint mobility, strengthen surrounding muscles, and improve range of motion. The intensity and duration of physical therapy sessions should be carefully managed by a qualified therapist to avoid exacerbating the injury and promote safe and effective recovery. Proper rehabilitation, including hand therapy, is essential to regain full function and prevent long-term limitations.
Rehabilitation and Return to Function
Pre-Rehabilitation Phase
This initial phase focuses on the stabilization and initial healing of the fractured bone. Crucially, the primary goal is to prevent further injury and promote a healthy environment for bone repair. This involves careful immobilization, pain management, and close monitoring of the fracture site. The medical team will carefully assess the patient's condition, including pain levels, swelling, and any potential complications. This phase is often characterized by a period of rest and recovery, allowing the body to focus on the healing process without undue strain.
Detailed assessments, including X-rays and physical examinations, will be conducted regularly to monitor healing progress and adjust treatment plans as needed. The patient's physical and emotional well-being are also considered, as these factors play a significant role in the overall recovery process. This early stage sets the foundation for successful rehabilitation and return to function.
Pain Management and Symptom Relief
Effective pain management is paramount throughout the entire rehabilitation process. Chronic pain can hinder the patient's ability to participate in rehabilitation exercises and activities, potentially delaying the return to function. A multi-faceted approach to pain management is often employed, combining medication, physical therapy modalities like heat and ice, and other techniques to alleviate discomfort and promote relaxation. This proactive management of pain is crucial for the patient's comfort and engagement in the rehabilitation process.
The medical team will work closely with the patient to develop a personalized pain management strategy, taking into account individual factors such as the location and severity of the fracture, the patient's pain tolerance, and any potential allergies or sensitivities to medications. This individualized approach ensures the most effective and safe pain relief possible.
Restorative Exercises and Mobility
As the fracture begins to heal, the focus shifts to restoring mobility and strength. This involves a gradual introduction of controlled exercises designed to improve range of motion, flexibility, and muscle strength around the affected area. These exercises are carefully calibrated to avoid putting undue stress on the healing bone. The progression of exercises is crucial, moving from simple range-of-motion exercises to more complex strength training activities as the bone heals and the patient demonstrates improvement.
Professional guidance from physical therapists is essential in this phase. They will provide personalized exercise plans, ensuring that the exercises are appropriate for the patient's specific needs and recovery progress. The goal is to gradually increase the intensity and duration of the exercises, building back strength and function without jeopardizing the integrity of the healing bone.
Functional Training and Return to Activity
Once the bone has healed adequately, the focus transitions to functional training. This involves exercises and activities that mimic the everyday movements and tasks the patient needs to perform. This phase is critical for restoring the patient's ability to perform daily activities without pain or limitations. The goal is to gradually increase the complexity and intensity of the activities, ensuring that the patient can safely and effectively return to their desired level of function.
This stage often involves working with occupational therapists, who can assess the patient's needs in relation to their home environment and work or school activities. They can provide modifications or adaptive equipment to support the patient's return to normal activities. The ultimate aim is to ensure a safe and successful return to their pre-injury lifestyle.
Monitoring and Long-Term Management
Even after the patient has returned to full function, ongoing monitoring and long-term management are crucial for preventing complications and ensuring long-term well-being. This involves regular check-ups, assessments, and ongoing support from the medical team. The patient should be educated on strategies to maintain bone health and prevent future injuries. This preventative approach is vital in promoting long-term recovery and reducing the risk of re-injury.
The long-term management plan may also include recommendations for lifestyle adjustments, such as dietary changes to support bone health, and guidance on activities that could potentially re-traumatize the healing bone. This proactive approach ensures that the patient is well-prepared for a sustained, healthy lifestyle following bone fracture recovery.