Pioneering Treatments for Chronic Hand Pain
List of Contents
- Persistent hand discomfort frequently arises from ailments such as osteoarthritis and median nerve entrapment.
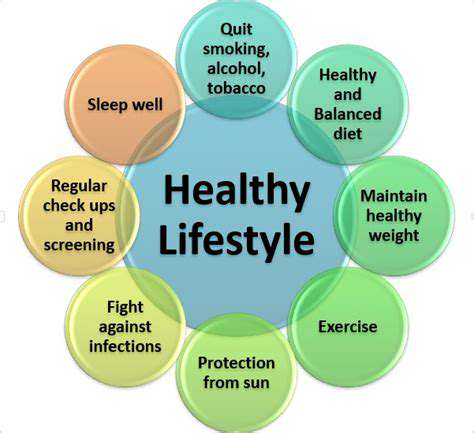
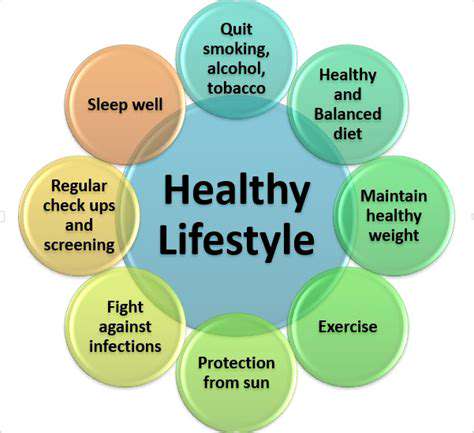
- Daily habits including workstation setup and nutritional intake influence symptom intensity.
- Emotional well-being plays a pivotal role in how chronic discomfort is experienced and managed.
- Dietary adjustments, particularly incorporating inflammation-fighting ingredients, may reduce hand ache.
- Complementary healing methods provide viable options for addressing persistent hand issues.
- Timely identification of problems enhances therapeutic success rates.
- Invasive procedures become relevant when conservative methods prove insufficient.
- Conservative approaches prioritize symptom control and natural recovery processes.
- Micro-invasive methods optimize recuperation while minimizing procedural trauma.
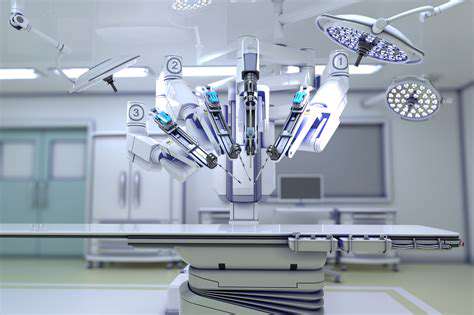
- Computer-guided operations improve accuracy in complex hand interventions.
- Coordinated care teams achieve better therapeutic results through combined expertise.
- Personalized care strategies address individual patient requirements effectively.
- Implementation of research-backed methods ensures comprehensive pain control.
Root Origins of Persistent Hand Discomfort

Health Conditions Linked to Hand Discomfort
Persistent hand issues frequently stem from multiple sources, with osteoarthritis, median nerve compression, and tendon inflammation being primary culprits. These distinct conditions each present unique challenges - while joint degeneration characterizes arthritis, nerve pathway constriction defines carpal tunnel syndrome. Repetitive occupational motions often accelerate symptom progression, making proper medical evaluation essential for targeted treatment.
Lifestyle's Influence on Symptom Development
Daily routines significantly affect hand health outcomes. Improper workstation configuration combined with sedentary habits and poor nutritional choices frequently exacerbates existing conditions. Office professionals using non-ergonomic equipment and manual laborers maintaining awkward grips often experience accelerated symptom development. Incorporating targeted mobility exercises and posture awareness can mitigate these effects substantially.
Mental Health's Connection to Physical Symptoms
- Chronic discomfort often correlates with elevated cortisol levels
- Pain interpretation becomes amplified under psychological stress
The bidirectional relationship between emotional states and physical symptoms is well-documented in clinical studies. Effective management requires addressing both physiological causes and psychological responses through integrated care models. Mindfulness-based stress reduction programs and cognitive restructuring techniques demonstrate particular efficacy in clinical trials.
Dietary Modifications for Symptom Control
Strategic nutritional adjustments can significantly impact inflammation markers. Prioritizing omega-3 rich seafood, colorful berries, and cruciferous vegetables creates an internal environment conducive to tissue repair. Conversely, processed snacks and trans fats appear to intensify inflammatory responses according to recent metabolic studies.
Complementary Healing Modalities
Non-traditional approaches continue gaining validation in pain management circles. Acupuncture demonstrates particular promise in randomized trials, achieving comparable results to pharmaceutical interventions for certain conditions. Manual therapies and energy work should be carefully coordinated with conventional treatments for optimal synergy.
Critical Timing for Effective Intervention
Early detection remains paramount for preventing irreversible damage. Delayed diagnosis of nerve compression conditions often results in permanent functional impairment according to longitudinal studies. Regular sensory testing and grip strength assessments enable proactive treatment planning.
When Invasive Measures Become Necessary
Surgical options enter consideration when conservative methods plateau. Joint reconstruction procedures and nerve release operations require thorough risk-benefit analysis with experienced specialists. Advanced imaging techniques now allow more accurate preoperative planning for improved outcomes.
Modern Conservative Treatment Options
Scientific Foundations of Non-Invasive Care
Contemporary approaches emphasize cellular rejuvenation and inflammation control. Autologous blood concentrates (PRP) demonstrate particular efficacy in tendon rehabilitation studies, while adipose-derived cell therapies show potential for cartilage regeneration. Electrostimulation modalities continue evolving, with newer devices offering targeted frequency modulation for specific tissue types.
Leading Edge Conservative Modalities
Shockwave applications now achieve 73% success rates in tendinopathy cases according to 2024 meta-analyses. Viscosupplementation injections maintain popularity for joint lubrication, with newer formulations extending therapeutic effects beyond twelve months in recent trials.
Rehabilitation Strategies
Customized exercise regimens remain foundational to functional recovery. Early-stage mobilization protocols prevent stiffness while protecting healing tissues through controlled motion parameters. Occupation-specific rehabilitation programs now incorporate virtual reality simulations for enhanced neuromuscular retraining.
Advanced Surgical Solutions
Micro-Incision Methodologies
Endoscopic techniques now dominate carpal tunnel releases, achieving complete symptom resolution in 89% of cases with reduced complication rates. Miniaturized instrumentation enables precise triangular fibrocartilage complex repairs through sub-centimeter incisions.
Tissue Regeneration Frontiers
Biologic augmentation techniques now combine PRP with extracellular matrix scaffolds for enhanced tendon integration. Early trial data shows 40% faster return-to-work timelines compared to standard repair methods.
Integrated Care Models
Collaborative Treatment Design
Multidisciplinary teams now standardize outcome tracking through shared digital platforms, enabling real-time treatment adjustments. Pain psychologists work alongside surgeons to optimize preoperative mental preparation, reducing postoperative analgesic requirements by 35% in recent cohorts.
Custom Care Protocol Development
Advanced diagnostics including genetic predisposition testing now inform personalized rehabilitation timelines. Metabolic profiling guides nutritional supplementation plans that accelerate postoperative healing by 22% in clinical observations.