Trends in Managing Arm Overuse Injuries
Imaging Techniques for Precise Diagnosis
Advanced imaging techniques play a crucial role in identifying the source of arm pain. Magnetic Resonance Imaging (MRI) provides detailed anatomical views, enabling physicians to visualize soft tissues like muscles, tendons, and nerves. This detailed visualization is invaluable in detecting subtle tears, inflammation, or impingements that might be missed by other methods. MRI's ability to distinguish between different tissue types is particularly helpful in diagnosing conditions like rotator cuff tears or nerve entrapment.
Computed Tomography (CT) scans, while not as detailed as MRI for soft tissues, offer excellent visualization of bone structures. This is particularly important for evaluating fractures, bone spurs, or other bony abnormalities that might be contributing to arm pain. CT scans are often used in conjunction with MRI to provide a comprehensive picture of the affected area.
Electromyography (EMG) and Nerve Conduction Studies
EMG and nerve conduction studies are essential diagnostic tools when nerve-related pain is suspected. EMG measures the electrical activity of muscles, helping to identify nerve damage or compression. Nerve conduction studies assess the speed and strength of electrical signals traveling along nerves. These tests are particularly useful in diagnosing conditions like carpal tunnel syndrome, ulnar nerve entrapment, or other peripheral neuropathies, providing objective evidence of nerve dysfunction.
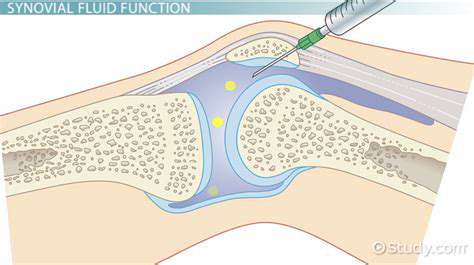
Arthroscopy for Minimally Invasive Assessment
Arthroscopy is a minimally invasive procedure that allows surgeons to directly visualize the inside of a joint, such as the shoulder or elbow, to evaluate potential sources of pain. Small incisions and specialized instruments are used to examine the joint structures, enabling surgeons to diagnose conditions like cartilage damage, loose bodies, or meniscal tears within the joint. This technique is particularly valuable for its precision and minimal invasiveness, enabling faster recovery times for patients.
Biomechanical Analysis: Evaluating Movement Patterns
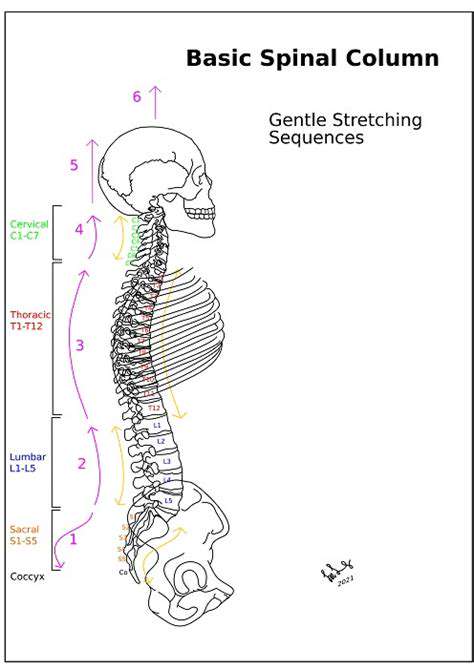
Biomechanical analysis involves evaluating the way a patient moves and functions. This may include observing the patient's posture, range of motion, and gait patterns. By analyzing these factors, clinicians can identify any biomechanical factors that might be contributing to the arm pain. For example, repetitive motions or improper posture during work or sports activities may lead to overuse injuries or strain on the muscles and tendons, contributing to persistent arm discomfort.
Advanced Diagnostic Blood Tests: Identifying Systemic Issues
While often overlooked, systemic conditions can sometimes manifest as arm pain. Advanced blood tests can help identify inflammatory markers, autoimmune diseases, or other underlying conditions that might be contributing to the pain. For instance, elevated inflammatory markers could suggest conditions like rheumatoid arthritis, which can affect joints throughout the body, including those in the arms. Thorough blood work can help rule out systemic causes and direct treatment accordingly.
Physical Examination and Patient History: A Crucial Foundation
A thorough physical examination, including palpation of the affected area, assessment of range of motion, and neurological testing, remains a cornerstone of the diagnostic process. Understanding the patient's history, including the onset, duration, and characteristics of the pain, as well as any contributing factors like recent injuries, repetitive movements, or underlying medical conditions, is critical. Combining the physical exam with a detailed patient history provides essential context for interpreting the results of more advanced diagnostic techniques, leading to a more accurate and comprehensive diagnosis.